Results From the FIDELITY Pooled Analysis
A review of results from the FIDELITY pooled analysis analyzing finerenone’s impact on cardiorenal morbidity and mortality in patients with type 2 diabetes and CKD.
Episodes in this series

Transcript:
Rajiv Agarwal, MD, MS: Before I tell you the results, I can tell you that when you look at the pooled data, this is not your usual patient you might see in the clinic. This is an incredibly well-treated population of a high-risk patient group. They all have type 2 diabetes and chronic kidney disease [CKD], with an age of 65 on average. The median duration of diabetes was 15 years, glycated hemoglobin was 7.7%, blood pressure was 137/76 mm Hg, and 46% of patients had a history of cardiovascular disease. Heart failure, not enriched, was 7.7%. Remember, we excluded people with symptomatic HFrEF [heart failure with reduced ejection fraction] … Statins were used in 72% of patients, and GLP-1 and SGLT2 inhibitors were used in about 7% of patients. We are looking at a benefit on top of this ideally treated group of patients, not a poorly treated group of patients.
If we were to look at a poorly treated group of patients, I would expect that the benefit would be even larger. Imagine you have a lot of albuminuria, a lot of heart failure, a lot of blood pressure: you might see an effect that is even larger. Forty percent of patients in the FIDELITY analysis had an eGFR [estimated glomerular filtration rate] of more than 60. Now that means that if you are simply looking at eGFR to diagnose chronic kidney disease, you have to change your practice. You’ll miss 40% of the patients who are otherwise eligible for finerenone because you never checked for albuminuria. If they have albuminuria, they’re eligible for participating in the trial, and 40% of patients were in the eGFR silent zone. Their creatinine’s not elevated, and you‘re not going to detect them as having CKD unless you look at the urine and figure out the UACR [urine albumin-to-creatinine ratio].
The mean eGFR in this population is actually 57.6. This is a very well preserved eGFR, but we have a broad characterization of patients. A third of the patients have an eGFR of less than 45. A quarter of the patients have an eGFR between 45 and 60. You have a very broad range of patients who participated in this study, and what we see is a reduction in cardiovascular death, nonfatal MI [myocardial infarction], nonfatal stroke, and hospitalization for heart failure by 14%. The P value is .0018, and the NNT [number needed to treat] after 3 years is 46. If you look at the kidney end point, which is the 57% composite, we have a 23% reduction in relative risk with a P value of .0002, and NNT after 3 years is 60. They were very respectable numbers regarding these events as seen in the FIDELITY analysis. It adds to a growing pool of data showing that you can indeed impact cardiovascular and kidney failure outcomes across a broad range of eGFRs and albuminuria to prevent both cardiovascular disease and kidney failure risk.
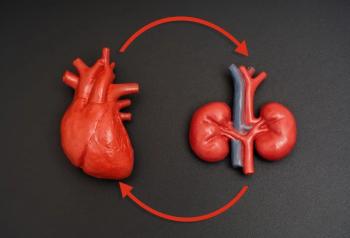
In other words, it’s never too early to start. If you have albuminuria, you can start. You can start as late as an eGFR of 25 or more, provided the potassium is 5 mmol/L or less. It’s a very broad population of patients you can treat. For the first time, we’re demonstrating that it can protect the heart and the kidneys together in this composite analysis.
Transcript edited for clarity.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.