- January 2024
- Volume 30
- Issue 1
- Pages: SP72-SP73
Next Frontier of Precision Hematology Uses Patient Tissue to Find a Therapy Match

Today, precision medicine in cancer care works like this: genomic testing, preferably next-generation sequencing (NGS), is used to find mutations or lesions that could be therapeutic targets. If results reveal the cause of cancer progression, and if there’s a therapy known to block this signal, patients can give the drug a try.
But often, it’s not so simple. Patients’ genomic makeup is heterogeneous, so what seems like a match on paper may not work in the body. Some patients may have multiple mutations in play at once. And if too few people have a given disease, it may be impossible to recruit enough patients for a clinical trial to confirm drug targets, even if a therapy seems promising.
Now some scientists are turning this precision medicine approach on its head: Instead of studying a given therapy in multiple patients, they start with the individual and examine how their cancer might respond to dozens of treatments—using the patient’s own tissue as the guide. With techniques called functional screening, investigators can link cancerous tissue to therapies that will likely produce results or rule out those that won’t.
The symposium “Multi-omics Driven Precision Hematology” explored this concept during the 65th American Society of Hematology Annual Meeting and Exposition in San Diego, California. This approach is a long time coming, explained session chair Pamela Becker, MD, a principal investigator in hematological malignancies at City of Hope, who described the skepticism within her own institution when she first pursued this research. But machine learning is changing things, and Becker appeared with 2 panelists equally engaged with these advances: Jun J. Yang, PhD, vice chair, Department of Pharmacy and Pharmaceutical Sciences, St. Jude Children’s Research Hospital; and Mika Kontro, MD, PhD, of Helsinki University Hospital and Institute for Molecular Medicine in Finland.
Drug sensitivity testing, Becker explained, reveals each patient’s unique patterns of sensitivity or resistance to various molecules, so that a clinician can gauge before therapy is administered how that individual’s tumor will respond. “Our vision of the future of precision hematology includes directing multi-omics studies and multi-omics including genomics, epigenomics, transcriptomics, proteomics, metabolomics,” she said.
Functional screening “will need to use computational biology methods which have become quite sophisticated, including machine learning, which we hope to translate rapidly to the clinic,” Becker said. “Our aim is to optimize survival for each patient.”
Beyond Next-Generation Sequencing
NGS has value, Yang said, but it also has limits. The current paradigm is a “linear” model in which a patient must have a known target that can be treated with a known therapy. And in cases such as chronic myeloid leukemia, there have been great successes.
“But this linear relationship holds true only for small number of patients,” he said. “Either the patient does not have a targetable mutation, or lesion, or the relationship between genetic mutation and drug response is not necessarily linear. It’s a lot more complicated than that.”
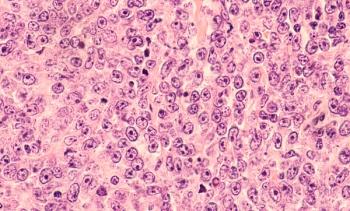
Yang used acute lymphoblastic leukemia (ALL), often seen in young children, to highlight the need for and possibilities of a multi-omics approach. ALL has about 3500 annual pediatric diagnoses and 6400 overall in the United States,1 but it has many subtypes. “Over the past 20-something years, we have made tremendous progress in terms of understanding the genetic complexity of this particular blood cancer,” he said, and investigators have delineated “23 different molecular subtypes, defined by translocation, gene expression, mutation, and so forth.”
Not all subtypes have targets, although some do, such as patients who are BCR-ABL positive, he said. “So, the big question is, how do we come back to the heterogeneity within ALL in terms of the genomic landscape to the heterogeneity of the treatment response, especially to different drugs?”
To address this, Yang and colleagues are constructing a “gene-drug map,” which he said will be a blueprint of ALL drugs in all pediatric and adult indications. So far, the project has culled data from 1300 cases of relapsed or refractory ALL, gleaning 67,000 data points. The question now, he said, is how well testing of tissue, or “ex vivo” testing, works in predicting drug sensitivity.
Based on data gathered so far, Yang was able to offer examples of how this works. A collaboration between St. Jude’s and the Children’s Oncology Group found that patients’ sensitivity to dasatinib (Sprycel) strongly correlated with their BCL-ABL fusion status. About 20% of pediatric patients and about 29% of adult patients are sensitive to dasatinib, Yang said; of the cases that were sensitive to dasatinib, 73% were positive for BCR-ABL. “So, our positive control works very well.”
Delving further, the collaborators identified cases of patients where the overlap of mutations would make it impossible to use one, such as RAS, to stratify care in the conventional way—and drug sensitivity tests bore this out. He shared a case where use of minimal residual disease testing tracked a patient’s high level of disease prior to and after treatment; dasatinib was identified in drug sensitivity testing, resulting in remission that has lasted more than 2 years.
Role in Drug Development
Functional precision medicine has a role in drug development, Yang said. He reviewed a study that appeared in Leukemia involving the novel target LCK, present in 40% of T-cell ALL cases. Both dasatinib and ponatinib in block LCK with positive results, and Yang and collaborators evaluated the pharmacokinetics (PK) and pharmacodynamics (PD) of both drugs in patients with LCK-activated T-cell ALL, with ponatinib being more potent.2 Yang explained how research found that LCK and BCL2, the target of venetoclax, are activated at different stages, with a “totally inverse correlation between BCL2 and LCK,” and the varying activity of genetic lesions to block cell development, known as differentiation arrest, is what drives drug sensitivity in AML. In Leukemia, authors state their PK/PD profiles provide “critical data for the development of human trials of these agents.”2
Functional Screening in AML
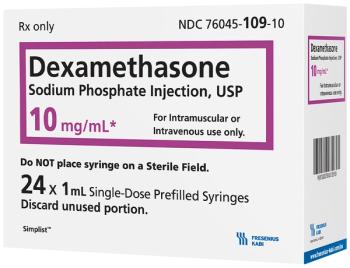
Among other studies, Kontro shared data from the ongoing phase 2 VenEx trial (NCT04267081) to highlight the predictive value of ex vivo drug sensitivity testing in acute myeloid leukemia (AML). In this trial, patients with AML receive testing to determine sensitivity to venetoclax. First results from this study, published in Haematologica, found that sensitivity testing was not only feasible in nearly all patients but also highly predictive of survival.3 Kontro’s update for 104 patients was consistent with the initial findings, which found that 88% of participants who were found to be sensitive to venetoclax achieved a treatment response; the median survival for those ex vivo–sensitive to venetoclax was 14.6 months, compared with 3.5 months for those who were insensitive.3
Role in Rare Disorders
Becker offered background on the development of assays used in functional screening, and then outlined examples where it was used alongside molecular testing to find treatments for patients with rare disorders, such as myeloproliferative or myeloid neoplasm subtypes. In several cases, this approach was able to identify a treatment when the patient’s local physician had no clear options available.
Despite ongoing challenges in getting tissue to sites capable of this testing, as well as reimbursement, the panelists were hopeful. “Functional drug screening can provide possible drugs under combinations for any diagnosis that may provide benefit to individual patients with specific features,” Becker said.
References
1. Key statistics for acute lymphocytic leukemia (ALL). American Cancer Society. Updated January 12, 2023. Accessed January 4, 2024. https://bit.ly/3tFDsMS
2. Yoshimura S, Panetta JC, Hu J, et al. Preclinical pharmacokinetic and pharmacodynamic evaluation of dasatinib and ponatinib for the treatment of T-cell acute lymphoblastic leukemia. Leukemia. 2023;37(6):1194-1203. doi:10.1038/s41375-023-01900-5
3. Kuusanmaki H, Kytola S, Vanttinen I, et al. Ex vivo venetoclax sensitivity testing predicts treatment response in acute myeloid leukemia. Haematologica. 2023;108(7):1768-1781. doi:10.3324/haematol.2022.281692
Articles in this issue
about 2 years ago
Overcoming Barriers to Care Equity in Multiple Myelomaabout 2 years ago
ASH 2023: Coverage in MDS, Myeloproliferative Diseaseabout 2 years ago
ASH 2023: Coverage in Multiple Myelomaabout 2 years ago
ASH 2023: Coverage of ALLabout 2 years ago
ASH 2023: Coverage of cHLabout 2 years ago
ASH 2023: Coverage of MCLabout 2 years ago
ASH 2023: Coverage of CLL/SLLabout 2 years ago
ASH Abstracts Showcase Effective Treatments for MM, CLL, FLabout 2 years ago
Data Reveal Racial, SDOH Factors Linked to OS Differences in CLLNewsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.