- February 2025
- Volume 31
- Issue Spec. No. 2
- Pages: SP107-SP108
Banner Year for Bispecifics as Therapies Advance Into the Community Setting
Key Takeaways
- Bispecific antibodies offer outpatient treatment options, increasing access to advanced therapies in community settings and reducing the burden of travel for patients.
- Recent approvals and clinical trials show significant efficacy of bispecifics in multiple cancers, with notable improvements in survival and response rates.
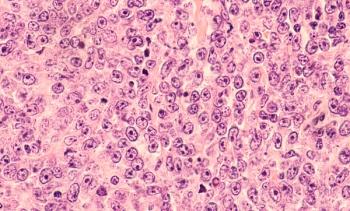
Patients with certain blood cancers such as multiple myeloma and leukemias often have to face a difficult choice: travel hundreds of miles to a major academic medical center for a month or more to receive a chimeric antigen receptor (CAR) T-cell therapy that could wipe out the disease, or stay local and receive a potentially less potent treatment.
For many patients, the distance, time away from home, and requirement for a caregiver companion are too burdensome.1 However, advances with bispecific antibodies, a different type of engineered immunotherapy that binds to 2 different targets simultaneously, are changing the equation. Unlike CAR T therapies, bispecifics can often be delivered in outpatient settings, expanding access to care for patients who might otherwise have foregone treatment.2 Because 85% of patients with cancer receive care in the community setting,3 clinicians have welcomed this advancement.
“The democratization of bispecifics and cellular therapies is essential to allowing all these patients to access the most cutting-edge therapies,” Michael Byrne, DO, hematologist/oncologist at Tennessee Oncology, said during Managed Care Cast, a podcast by The American Journal of Managed Care.4
“Those of us in community oncology are certainly capable of taking care of these patients either by ourselves or in partnership with a program or institution that can help navigate the early step-up doses with the goal of getting them back to their local clinics as quickly as possible for subsequent care.”
New Approvals
The year 2024 marked a notable expansion in this therapeutic class, with approvals of both new therapies and new indications for existing therapies (TABLE).5-9 These include: epcoritamab (Epkinly)5 for relapsed/refractory follicular lymphoma; tarlatamab (Imdelltra)6 for previously treated extensive-st age small cell lung cancer; zanidatamab (Ziihera)7 for previously treated unresectable or metastatic HER2-positive biliary tract cancer; zenocutuzumab (Bizengri)8 for previously treated non–small cell lung cancer and pancreatic adenocarcinoma with an NRG1 gene fusion; and blinatumomab (Blincyto)9 for consolidation in CD19-positive Philadelphia chromosome–negative acute lymphoblastic leukemia.
Real-world data presented at the 66th American Society of Hematology Annual Meeting and Exposition in December 2024 (ASH 2024) provided a first look at how quickly bispecific antibodies have been adopted in community oncology settings for multiple myeloma.2 After the FDA’s approval of teclistamab (Tecvayli) in late 2022, just 1 patient received this therapy compared with 148 on other treatments. Following the 2023 approvals of talquetamab (Talvey) and elranatamab (Elrexfio), usage grew to 45% of eligible patients, reaching 54% by mid-2024. Teclistamab dominated prescribing patterns in 91% of cases, with treatments distributed evenly across practices in the US.
Clinical and Development Updates
Several bispecific antibodies have reported clinical results and updates at recent medical meetings, business events, and industry conferences. Below is a snapshot of some of these developments.
Blinatumomab. Results from a pivotal phase 3 trial (NCT03914625) presented at ASH 2024 and published in The New England Journal of Medicine showed that adding blinatumomab to standard chemotherapy significantly improved outcomes, achieving a 3-year disease-free survival rate of 96% vs 88% with chemotherapy alone. Among Hispanic children, who historically face worse outcomes in leukemia care, blinatumomab extended disease-free survival by an additional 150 days.10
Teclistamab and talquetamab. At the 21st International Myeloma Society Annual Meeting (IMS 2024), investigator Yael Cohen, MD, head, Myeloma Unit, Tel Aviv Sourasky Medical Center, presented updated results from the phase 1b RedirecTT-1 study (NCT04586426).11 The study evaluated a combination of teclistamab and talquetamab and reported an overall response rate of 80%, with 52% of patients achieving a complete response or better. The combination also demonstrated an 18-month progression-free survival rate of 70% and a duration of response rate of 86% at 18 months.
“Both of these agents are best-in-class bispecifics. They’re performing very well from a competitive share standpoint,” Jennifer Taubert, executive vice president and worldwide chairman of innovative medicine at Johnson & Johnson, said during the company’s earnings call on January 22.12 “We’ve got them…being utilized in the academic setting, and we’re working that out into more of the community setting, which will be important for their continued growth and uptake.”
Epcoritamab. Granted an accelerated approval in 2023 to treat relapsed/refractory diffuse large B-cell lymphoma (DLBCL), epcoritamab has demonstrated strong efficacy in previously untreated DLBCL. Data presented at ASH 2024 showed that combining epcoritamab with R-CHOP (rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, prednisone) chemotherapy in untreated high-risk DLBCL achieved a 100% response rate and 87% complete response rate,13 with 83% of complete responders remaining in remission at 24 months. Data presented in May 2024 at the American Society of Clinical Oncology (ASCO) Annual Meeting showed that in previously untreated follicular lymphoma, when combined with rituximab and lenalidomide, epcoritamab delivered a 95% response rate and 85% complete response rate.14
Glofitamab. Marketed as Columvi, this bispecific antibody that targets CD20 on B cells and CD3 on T cells received accelerated approval15 in June 2023 for patients with DLBCL who had received 2 or more prior systemic therapies. Phase 3 trial results (NCT04408638)16 which were reported at the European Hematology Association Congress in June 2024, showed that combining glofitamab with chemotherapy doubled survival for these patients at 26 months vs 13 months with standard therapy. The combination achieved higher complete response rates (59% vs 25%) and longer progression-free survival (14 vs 3.6 months). Additional studies in mantle cell lymphoma also showed strong responses. Notably, glofitamab is administered as a fixed-duration intravenous infusion over approximately 8.5 months, offering a time-limited treatment option.
Ivonescimab. This investigational bispecific antibody targeting PD-1 and VEGF is the first therapy to show a statistically significant improvement over pembrolizumab (Keytruda) in a head-to-head phase 3 HARMONi-2 trial17 called for PD-L1–positive non–small cell lung cancer. Beyond lung cancer, phase 2 data indicate promising efficacy in advanced triple-negative breast cancer, colorectal cancer, and head and neck squamous cell carcinoma, achieving response rates of up to 85% with a manageable safety profile.18
“Ivonescimab is effectively a unique mechanism of action from anything developed historically,” Maky Zanganeh, DDS, co-CEO and president of Summit Therapeutics, told attendees at the 43rd Annual J.P. Morgan Healthcare Conference on January 13. “Ivonescimab will continue to be rapidly tested, and its development advanced way beyond non–small cell lung cancer.”
Trispecific Antibodies
The next wave of therapies adds another element to create trispecific antibodies, which target 3 different antigens. Merck has made significant investments in this space by acquiring Harpoon Therapeutics in 2024 for $680 million19 and gaining access to MK-6070, a trispecific T-cell engager targeting DLL3 in small cell lung cancer. The company also acquired Eyebiotech Limited,20 securing Restoret, a trispecific for nononcology indications such as age-related macular degeneration and diabetic macular edema. The company is exploring combinations of trispecifics with other modalities, partnering with Daiichi Sankyo to add an antibody-drug conjugate in solid tumor trials.21
Johnson & Johnson is also experimenting with a trispecific combination targeting B-cell maturation antigen, GPRC5D, and CD3. Preclinical studies presented at ASH 2023 suggest that this approach could reduce antigen escape and improve immune-mediated tumor destruction.22 A presentation at IMS 2024 reviewed progress on this trispecific, known as JNJ-7965322, which essentially combines the targets of teclistamab and talquetamab but does so with much less toxicity.23
A Robust Pipeline
The pipeline for these therapies continues to expand, with multiple drugs in late-stage development. A Nature Reviews Drug Discovery report24 from March 2024 estimates more than 200 bispecifics were in clinical development at that time, with approximately half in phase 2 or 3 trials or already approved. These therapies target both hematologic malignancies and solid tumors, with T-cell engagers and immunomodulatory mechanisms dominating the field. Looking ahead, nearly 30 antibody-based therapies are under regulatory review globally, with 18 additional therapies expected to submit marketing applications by the end of 2025, including bispecific and trispecific treatments.25
“In the next few years, we’re likely to see [a] waterfall of new approvals, whether it be new drugs altogether, combination therapies, [or] therapies moving into earlier lines,” said Tyler Sandahl, PharmD, of Mayo Clinic, said during an interview with Managed Care Cast.4 “We just need to stay vigilant…and support our patients the best we can.”
Limitations
Although bispecific and trispecific antibodies offer new treatment options for patients, their clinical use is not without challenges. Unlike CAR T therapies, which are administered as a single infusion with potentially curative outcomes, bispecifics and trispecifics require frequent dosing—often weekly or biweekly infusions over an extended period. This ongoing treatment burden can be particularly taxing for patients who must regularly travel to infusion centers, especially those in rural or underserved areas.
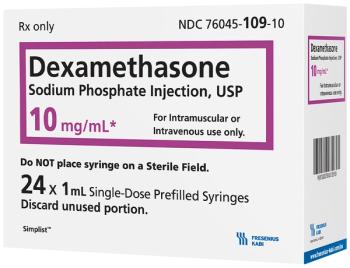
Despite these differences, there are currently no consensus guidelines tailored specifically to bispecific antibodies, according to a 2024 report published in Blood.26 Instead, management strategies are often adapted from protocols developed for CAR T therapies. The report recommended an approach that focused on proactive preparation, such as baseline testing and premedications, alongside patient and caregiver education to monitor for symptoms.
Practical Lessons for Clinicians
ASCO outlined some of the key steps clinicians need to be aware of when managing bispecific toxicities.27 such as inpatient monitoring for teclistamab and talquetamab during dose escalation, unlike mosunetuzumab (Lunsumio), which can be administered in an outpatient setting. The article noted that collaborative care models, where community oncologists partner with academic centers for early treatment phases, can be critical for ensuring safety during higher-risk periods. Ensuring that clinicians and staff are up to date on the latest efficacy and safety data is also important, the article notes, as patients often rely on online resources (44%) and support groups (38%) for information about these therapies.
“By surmounting barriers to access and investing in the education of both providers and patients, the oncology community is paving the way for a future where advanced cancer treatments are accessible to all who need them, irrespective of their geographic or economic circumstances,” the ASCO article authors wrote. “The future of oncology care hinges not only on the development of novel therapies but also on the ability of our health care systems to adapt and provide these therapies to all patients in need.”
References
1. Flinn R. Miles matter: the geographic disparity that impacts access to CAR T therapy. The American Journal of Managed Care. October 13, 2024. Accessed January 25, 2025. https://www.ajmc.com/view/miles-matter-the-geographic-disparity-that-impacts-access-to-car-t-therapy
2. Herms L, Su Z, Paulus J, Zackon I. Real-world utilization of bispecific antibodies for treatment of relapsed/refractory multiple myeloma in the US community oncology setting. Blood. 2024;144(suppl 1):2410. doi:10.1182/blood-2024-208825
3. Bringing research to the community to reduce cancer disparities. National Cancer Institute. September 21, 2027. Accessed January 23, 2025. https://www.cancer.gov/research/areas/disparities/chanita-hughes-halbert-clinical-trials-community-access
4. Caffrey M, Joszt L. Operationalizing bispecifics in multiple myeloma. The American Journal of Managed Care. November 27, 2024. Accessed January 24, 2025. https://www.ajmc.com/view/operationalizing-bispecifics-in-multiple-myeloma
5. FDA grants accelerated approval to epcoritamab-bysp for relapsed or refractory follicular lymphoma. FDA. June 26, 2024. Accessed January 24, 2025. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-epcoritamab-bysp-relapsed-or-refractory-follicular-lymphoma
6. FDA grants accelerated approval to tarlatamab-dlle for extensive stage small cell lung cancer. FDA. May 16, 2024. Accessed January 23, 2025. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-tarlatamab-dlle-extensive-stage-small-cell-lung-cancer
7. FDA grants accelerated approval to zanidatamab-hrii for previously treated unresectable or metastatic HER2-positive biliary tract cancer. FDA. November 20, 2024. Updated November 21, 2024. Accessed January 23, 2025. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-zanidatamab-hrii-previously-treated-unresectable-or-metastatic-her2
8. FDA grants accelerated approval to zenocutuzumab-zbco for non-small cell lung cancer and pancreatic adenocarcinoma. FDA. December 4, 2024. Accessed January 23, 2025.https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-zenocutuzumab-zbco-non-small-cell-lung-cancer-and-pancreatic
9. FDA approves blinatumomab as consolidation for CD19-positive Philadelphia chromosome-negative B-cell precursor acute lymphoblastic leukemia. FDA. June 14, 2024. Accessed January 20, 2025. https://bit.ly/3Em8EFO
10. Gupta S, Rau RE, Kairalla JA, et al. Blinatumomab in standard-risk B-cell acute lymphoblastic leukemia in children. N Engl J Med. Published online December 7, 2024. doi:10.1056/NEJMoa2411680
11. Cohen YC, Magen H, Gatt M, et al. Talquetamab + teclistamab in patients with relapsed/refractory multiple myeloma: updated phase 1b results from RedirecTT-1 with >1 year of follow-up. Presented at: 21st International Myeloma Society (IMS) Annual Meeting; September 25-28, 2024; Rio de Janeiro, Brazil. Accessed January 24, 2025. https://www.jnjmedicalconnect.com/media/attestation/congresses/oncology/2024/ims/talquetamab-tal-teclistamab-tec-in-patients-pts-with-relapsedrefractory-multiple-myeloma-rrmm-update.pdf
12. Johnson & Johnson (JNJ) Q4 2024 earnings call transcript. Motley Fool. January 22, 2025. Accessed January 23, 2025. https://www.fool.com/earnings/call-transcripts/2025/01/22/johnson-johnson-jnj-q4-2024-earnings-call-transcri/
13. Falchi L, Offner F, de Vos S, et al. Fixed-duration epcoritamab + R-CHOP induces high complete response rates in patients with previously untreated diffuse large B-cell lymphoma with high-risk features: long-term results from the EPCORE NHL-2 trial. Blood. 2024;144(suppl 1):581. doi:10.1182/blood-2024-198023
14. Lori LA, Falchi L, Vermaat JSP, et al. Epcoritamab with rituximab + lenalidomide (R2) in previously untreated (1L) follicular lymphoma (FL) and epcoritamab maintenance in FL: EPCORE NHL-2 arms 6 and 7. J Clin Oncol. 2024;42(suppl 16):7014. doi:10.1200/JCO.2024.42.16_suppl.7014
15. FDA grants accelerated approval to glofitamab-gxbm for selected relapsed or refractory large B-cell lymphomas. FDA. June 15, 2023. Updated June 16, 2023. Accessed January 24, 2025. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-grants-accelerated-approval-glofitamab-gxbm-selected-relapsed-or-refractory-large-b-cell
16. Abramson J, Ku M, Hertzberg M, et al. Glofitamab plus gemcitabine and oxaliplatin (Glofit-GemOx) for relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL): results of a global randomized phase III trial (STARGLO). Presented at: European Hematology Association 2024 Congress; June 13-16, 2024; Madrid, Spain. Abstract LBA3438. https://library.ehaweb.org/eha/2024/eha2024-congress/4136516/jeremy.abramson.glofitamab.plus.gemcitabine.and.oxaliplatin.28glofit-gemox29.for.html
17. Ivonescimab monotherapy decisively beats pembrolizumab monotherapy head-to-head, achieves statistically significant superiority in PFS in first-line treatment of patients with PD-L1 positive NSCLC in China. News release. Summit Therapeutics Inc; May 30, 2024. Accessed January 25, 2025. https://www.smmttx.com/pressrelease/ivonescimab-monotherapy-decisively-beats-pembrolizumab-monotherapy-head-to-head-achieves-statistically-significant-superiority-in-pfs-in-first-line ca-treatment-of-patients-with-pd-l1-positive-nsclc-in/
18. Promising anti-tumor activity and safety of ivonescimab in combination therapies in CRC, TNBC, and HNSCC featured at ESMO 2024. News release. Summit Therapeutics Inc; September 16, 2024. Accessed January 25, 2025. https://www.smmttx.com/pressrelease/promising-anti-tumor-activity-and-safety-of-ivonescimab-in-combination-therapies-in-crc-tnbc-and-hnscc-featured-at-esmo-2024/
19. Merck completes acquisition of Harpoon Therapeutics, Inc. News release. Merck; March 11, 2024. Accessed January 25, 2025. https://www.merck.com/news/merck-completes-acquisition-of-harpoon-therapeutics-inc/
20. Merck completes acquisition of EyeBio. News release. Merck; July 12, 2024. Accessed January 25, 2025. https://www.merck.com/news/merck-completes-acquisition-of-eyebio/
21. Daiichi Sankyo and Merck enter into global development and commercialization agreement for MK-6070. News release. Merck; August 6, 2024. Accessed January 25, 2025. https://www.merck.com/news/daiichi-sankyo-and-merck-enter-into-global-development-and-commercialization-agreement-for-mk-6070/
22. Pillarisetti R, Yang D, Yao J, et al. Characterization of JNJ-79635322, a novel BCMAxGPRC5DxCD3 T-cell redirecting trispecific antibody, for the treatment of multiple myeloma. Presented at: 65th American Society of Hematology Annual Meeting & Exposition; December 9-12, 2023; San Diego, CA. https://ash.confex.com/ash/2023/webprogram/Paper174941.html
23. Caffrey M. From CARs to trispecifics, more choices to come in multiple myeloma.The American Journal of Managed Care. October 1, 2024. Accessed January 25, 2025. https://www.ajmc.com/view/from-cars-to-trispecifics-more-choices-to-come-in-multiple-myeloma
24. Klein C, Brinkmann U, Reichert JM, Kontermann RE. The present and future of bispecific antibodies for cancer therapy. Nat Rev Drug Discov. 2024;23(4):301-319. doi:10.1038/s41573-024-00896-6
25. Crescioli S, Kaplon H, Wang L, Visweswaraiah J, Kapoor V, Reichert JM. Antibodies to watch in 2025. MAbs. 2025;17(1):2443538, doi:10.1080/19420862.2024.2443538
26. Crombie JL, Graff T, Falchi L, et al. Consensus recommendations on the management of toxicity associated with CD3×CD20 bispecific antibody therapy. Blood. 2024;143(16):1565-1575. doi:10.1182/blood.2023022432
27. Braun A, Gouni S, Pulles A, Strati P, Minnema MC, Budde LE. Bispecific antibody use in patients with lymphoma and multiple myeloma. Am Soc Clin Oncol Educ Book. 2024;44(3):e433516. doi:10.1200/EDBK_433516
Articles in this issue
12 months ago
February 2025 Health Equity News12 months ago
“This Is Important Information to Get Out”Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.