
Policy
Latest News
Latest Videos
Podcasts
CME Content
More News

Infectious disease was hit hardest by funding cuts to NIH grant for clinical trials that did not align with the Trump administration's priorities.

Cuts to Medicaid could spell trouble for pediatric health, as millions of children rely on Medicaid to cover their hospital expenses.

One in 5 of the highest-revenue drugs of 2022 was exclusively approved for rare conditions, accounting for more than 7% of US pharmaceutical spending.

Experts say proposed pharmaceutical tariffs could raise drug prices, impacting patient access and health care budgets.

One-third of F32 grant recipients secure follow-up NIH K awards, fueling new biomedical discoveries and career growth.

To mark the 30th anniversary of The American Journal of Managed Care, each issue in 2025 includes a special feature: reflections from a thought leader on what has changed—and what has not—over the past 3 decades and what’s next for managed care. The November issue features a conversation with Laurie C. Zephyrin, MD, MPH, MBA, senior vice president for achieving equitable outcomes at the Commonwealth Fund. This interview has been edited for length and clarity.

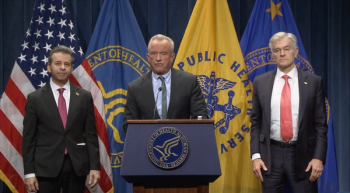
HHS has initiated removal of black box warnings on hormone replacement therapy, citing its advantages to women's health, but also drawing pushback.

In this investigation, the authors evaluated the impact of a voluntary transition to risk-based contracts under Medicare Advantage on health care use.

Oncology experts at PCOC 2025 discuss breakthrough therapies, AI-driven care, and evolving care delivery models shaping the future of oncology.
Explore how the WISeR Model addresses prior authorization reform, Medicare costs, and AI's role in tackling the health care affordability crisis.
Medicare Advantage plans that place greater restrictions on home health agency care delivery may have more adverse patient outcomes than plans that provide episodic payments.

Experts analyze how Trump's drug pricing policies, including Most Favored Nation (MFN) and tariffs, reshape pharma markets and impact patient costs and access.
AMCP Nexus connects pharmacy leaders, drives policy change, and empowers members to enhance health care access and improve patient outcomes.

Medbridge is working to refine remote therapeutic monitoring, or RTM, to transform physical therapy and enhance patient care.

Experts discuss personalized myasthenia gravis treatment, emphasizing patient education and engagement for optimal care and advocacy in managing this variable disease.

PBM legislation is rising nationwide, which experts emphasize could increase costs and hinder patient care.

Changing the FDA biosimilar interchangeability standards is a necessary but likely insufficient step to improve biosimilar competition in the US.

Geni Tunstall, JD, discusses how pharmacy benefit manager reforms, Medicaid changes, and the MAHA initiative may impact managed care pharmacy operations.
The FDA announced draft guidance to remove clinical efficacy studies for biosimilars and also issued the position that all biosimilars in the US should be interchangeable.

Premiums for coverage on the ACA marketplaces are set to jump by an average of 26% next year, even before the expiration of subsidies is factored in.

In the midst of a government shutdown, former House Speaker Paul Ryan urges clear policies, AI innovation, and patient-focused solutions to build a sustainable US health care system.

Discover how the Hearing Loss Association of America advocates for hearing loss awareness and hearing health integration through a dialogue with Barbara Kelley, executive director.

AI can transform health care by processing vast data, enhancing decision-making, and addressing biases, but needs remain for transparency and human oversight.

Ratna Kiran Bhavaraju-Sanka, MD, and Beth Stein, MD, advocate for improved proactive management of myasthenia gravis (MG) for better patient outcomes.

Panels held throughout the conference emphasized both how far the specialization has come but also how far it has yet to go.




















