
Myeloproliferative Neoplasms (MPN)
Latest News
Latest Videos

CME Content
More News

Besides Kent Hospital, the Association of Cancer Care Centers worked with Perlmutter Cancer Center at NYU Langone Hospital and Charleston Area Medical Center Vandalia Health in Charleston, West Virginia.

Perlmutter Cancer Center at NYU Langone was 1 of 3 sites to take part in the Association of Cancer Care Centers quality improvement initiative in myeloproliferative neoplasms (MPNs).

For several years, investigators have been studying combinations that include ruxolitinib, sold as Jakafi, to treat myeloproliferative neoplasms (MPNs).
A new study evaluating the quadratic phenotypic optimization platform shows it can accurately predict personalized drug combination sensitivities, paving the way for improved treatment strategies and outcomes in acute myeloid leukemia (AML).

The individual behavior of a patient’s myeloproliferative neoplasm (MPN) will determine how the disease is monitored and managed in the long term, explained Jennifer Vaughn, MD, of The Ohio State University Comprehensive Cancer Center.

While treatment options may be fairly straightforward for high-risk patients with polycythemia vera, it’s less clear for patients who are considered low risk, explained Jennifer Vaughn, MD.

Articles on myeloproliferative neoplasms (MPNs) covered the debate over how early to use cytoreductive therapies instead of phlebotomy in younger patients with polycythemia vera, the promise of vaccines, and the unmet potential of pegylated interferons.
A Yale School of Medicine team has created lists of criteria to help clinicians determine when next-generation sequencing (NGS) is appropriate for a patient with a myeloid neoplasm (MN), and when it is not.

Two posters presented at the 2024 American Society of Hematology meeting bolster evidence supporting the long-term clinical benefits of ruxolitinib for polycythemia vera and chronic graft-vs-host disease.

Research presented at the 66th American Society of Hematology Annual Meeting revealed that a genetic variant enriched in Andean populations, associated with reduced inflammation and improved response to ropeginterferon-α, could guide more precise treatments for polycythemia vera (PV) and essential thrombocythemia.

A decade after the discovery of CALR, the results are the first for a possible therapy for CALR-mutated MPNs to reach the clinic.
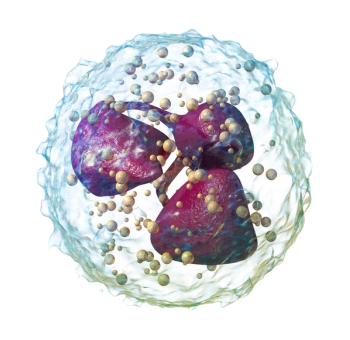
The key driver in both sets of findings is the relationship between neutrophils and inflammation.

Authors found the pharmacy costs for momelotinib were $11,095 higher per month, too much to offset higher transfusion costs for ruxolitinib.
Being married and having insurance can offer emotional support and financial stability to lead to early diagnosis and effective treatment, the authors found.
Experts are asking whether the study and treatment of myeloproliferative neoplasms (MPNs) is ready for a new era with new end points, with data that show how survival benefits are biologically linked to changes in the spleen, reduction in fibrosis, or other responses.

There can be a delay in diagnosis of myeloproliferative neoplasms as the symptoms of the diseases can be variable and common, such as fatigue, migraines, and difficulty concentrating, explained Ruben Mesa, MD, of Atrium Health.

Investigators added more data to an analysis first published in 2020 and got the same result: ruxolitinib beats other treatments for polycythemia vera.

An August 2024 update to the National Comprehensive Cancer Network (NCCN) clinical practice guidelines for treatment of myeloproliferative neoplasms (MPN) calls puts a priority on clinical trials, even preferring them to FDA-approved therapies in some cases. Aaron Gerds, MD, MS, of Cleveland Clinic Taussig Cancer Institute discusses the updates and what's in the pipeline for MPN treatment.

A study based on a decade's worth of Korean insurance data found that use of direct oral anticoagulants (DOACs) to address atrial fibrillation and venous thromboembolism in patients with myeloproliferative neoplasms (MPNs) is effective, with acceptable bleeding risk.
Researchers from Bulgaria conduct an analysis of the potential for therapeutic vaccines in by comparing testing results for patients from their country with an international data set.
Inflammation and genetic mutations can drive cardiovascular complications in patients with myeloproliferative neoplasms, which include disorders such as polycythemia vera, essential thrombocythemia, and primary myelofibrosis.
A review by authors from China examines evidence involving different treatment approaches.

While the Dynamic International Prognostic Scoring System and bone marrow blasts may predict overall survival, the lack of certain mutations is also associated with a better prognosis for myeloproliferative neoplasm, unclassifiable (MPN-U).

The introduction of momelotinib to treat myelofibrosis with anemia can result in small savings due to reduced transfusion-related costs, according to a budget impact model.

Raajit Rampal, MD, PhD, of Memorial Sloan Kettering Cancer Center, discusses the potential of a disease-modifying therapy in polycythemia vera, treating high-risk vs low-risk patients, and emerging therapies in the pipeline.
















