Review Recommends Options for Pediatric Treatment of Clostridioides difficile Infection
Evidence is insubstantial for treatment of Clostridioides difficile infection (CDI), but authors of a review of available evidence provide recommendations for agents and testing.
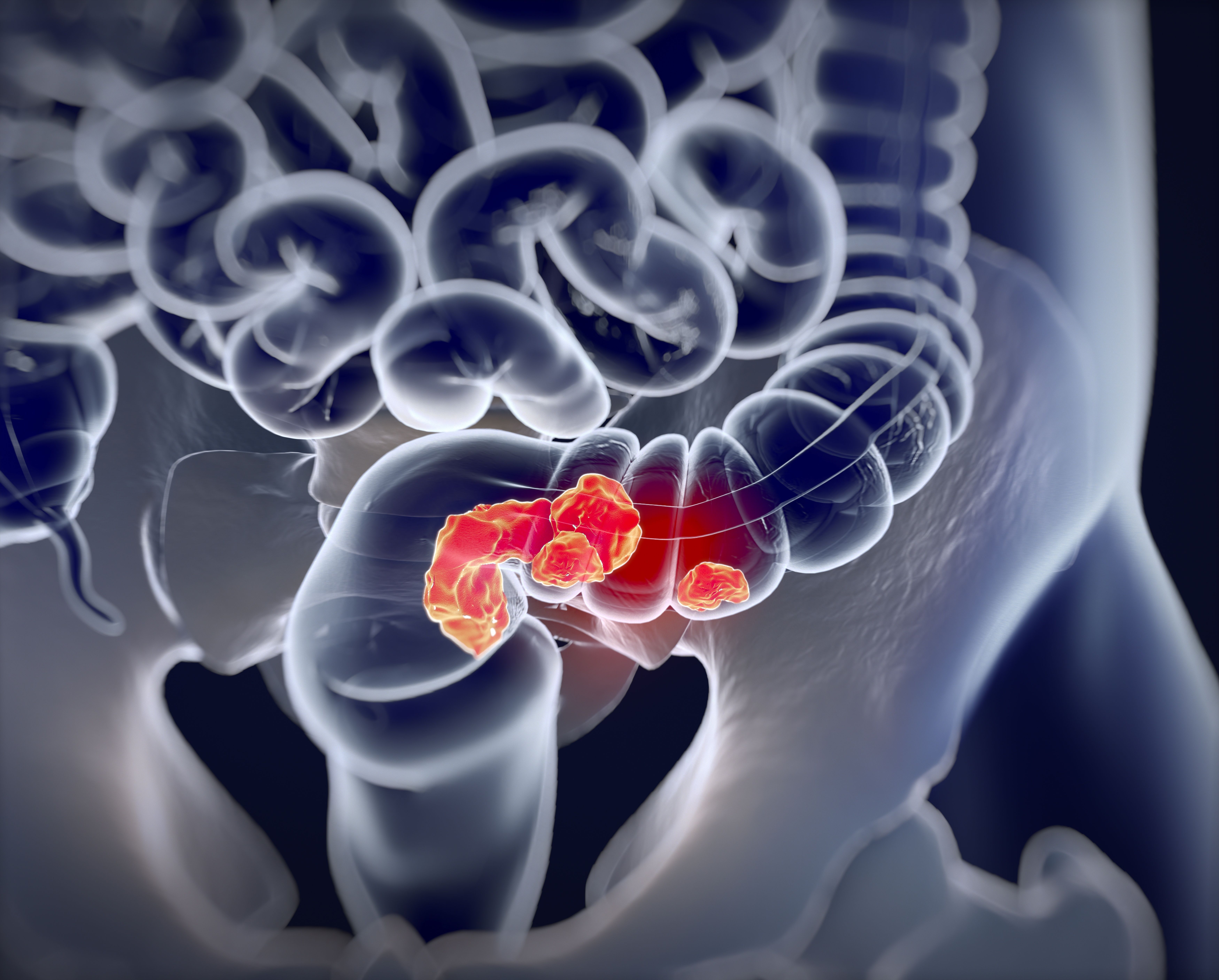
CDI produces toxins that bind to cell receptors and trigger apoptosis, or cell death, resulting in inflammation that causes diarrhea and colitis. “The management of pediatric CDI poses a challenge to health care providers due to lack of strong randomized controlled trials to guide pharmacological management,” the authors wrote.
They cited a concerning rise in the incidence of pediatric CDI hospitalizations from 3565 patients in 1997 to 7779 patients in 2006 (P < .001), although the incidence in the pediatric population is lower (24.2 per 100,000) than for all age groups (147.2 per 100,000), according to a 2015 study.
They attributed this rise to increased use of antibiotics, particularly cephalosporins and fluoroquinolones. Antibiotics alter the microbiota in the gastrointestinal tract, allowing for overgrowth of C. difficile and the development of CDI.
But despite this higher incidence in the pediatric population, there has been no commensurate increase in severity of cases, they wrote. “Significant efforts have been made by the Centers for Disease Control and Prevention to reduce the incidence of CDI and prevent the development of antibiotic resistance.”
The authors describe robust evidence available for treatment options in adult CDI, but said the reverse is the case for pediatric infections. That leads to questions whether treatments approved for adults are suitable for use in children, such as the oral vancomycin vs metronidazole in the front line for management of CDI.
Recommended Agents
In adults, oral vancomycin is recommended in this setting, but both agents are recommended for pediatric patients with an initial episode or first recurrence of CDI. However, metronidazole failure rates of 11% and 18% were observed in 2 studies of pediatric patients with CDI, and in the second of the studies, no failure was noted among patients who received oral vancomycin.
“These data suggest that metronidazole should not be used as the first line for an initial episode of severe CDI in pediatric patients,” the authors wrote. “Additional well-designed studies are needed to confirm this finding.”
The dosage recommendation for vancomycin in the pediatric population is 10 mg/kg 4 times daily with a maximum of 125 mg per dose, the authors wrote. That dosage is for patients with an initial episode or first recurrence of nonsevere disease. “On the basis of clinical data,” individual dosage can be increased to 500 mg in severe cases of CDI, they wrote.
Their review encompassed other agents. Fidaxomicin has previously been recommended only for adults, but a pediatric study found that 92% of patients had an early clinical response and 66% had a sustained response at 30 days. “Fidaxomicin was well tolerated in pediatric patients and the pharmacokinetic profile was very similar to that seen in adults with a high clinical response rate,” they wrote.
Fecal microbiota transplantation (FMT) has been highly successful in restoring normal microbiota in patients with CDI. However, the authors cautioned that special care is needed in applying FMT to pediatric treatment. “There is less evidence for use, more concern for adverse events, and fear of long-term outcomes when the microbiota is manipulated,” they wrote.
In addition, the FDA has cautioned about the development of multidrug-resistant organisms post FMT transplant. However, the authors recommended FMT be considered in pediatric CDI that is recurrent or develops following therapeutic failure after at least 1 course of vancomycin.
Other CDI Concerns in Pediatrics
There is no standard in pediatric treatment for knowing when to test for CDI during a series of diarrheal episodes. The Infectious Diseases Society of America recommends testing be considered “in those with unexplained and new-onset unformed stools at a frequency of at least 3 in a 24-hour period, although this is based on low-quality evidence.”
Another important concern is that CDI asymptomatic colonization (infection development) rates are higher in children (2%-50%) than in adults (3%-20%). In infants less than 1 month of age, colonization rates are as high as 37%; but in neonates and infants clinical CDI is rare because they do not have the cell receptors at that age that facilitate development of CDI, and so the authors did not recommend testing for CDI in patients 2 years and under.
Few studies have elucidated risk factors for CDI in pediatrics, they wrote. But it is possible to break the categories down into “modifiable risk factors” and “nonmodifiable risk factors.” In the former group is exposure to antibiotic agents.
“A recent study of pediatric patients in the inpatient and outpatient settings identified cephalosporins and clindamycin to be the most common antibiotics received within the 30 days before CDI diagnosis,” authors of the review wrote. Infections are more common among those who have received more than 1 class of antibiotic.
“Proton pump inhibitors and other suppressors of gastric acid have been documented to increase risk of CDI,” they wrote.
Nonmodifiable risk factors include comorbidities, such as transplants, pancreatitis, inflammatory bowel disease, and HIV. “Hospitalization has also been reported as a major risk factor for pediatric CDI across several studies, with nearly 50% of patients in some studies presenting with a history of hospitalization within the last month,” the authors wrote.
Reference
DeVine MN, MacBrayne CE, Child J, Blackmer AB. Pharmacological management of pediatric Clostridioides difficile infection: clarifying the controversies. J Pediatr Health Care. Published online August 17, 2021. doi:10.1016/j.pedhc.2021.06.005.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.