Payer Perspective of Anemia in CKD
A discussion on the health care resource utilization in a patient with anemia in CKD and the importance of monitoring hemoglobin levels for treatment.
Transcript
Peter L. Salgo, MD: All right. Let’s go to our payer, Dr Crittenden, who has distinguished us with his presence from the west coast. What percentage of your population with CKD [chronic kidney disease] ends up developing anemia? You’ve got all the good data; you’re the data collector here.
Stanley Crittenden, MD: That’s a good question. I’ll mirror what Bob said here. The prevalence of anemia increases as GFR [glomerular filtration rate] decreases, right? In your early stage III, you see single-digit percentages of people with anemia, so less than 5%. By the time you get to the later stages, like IIIB, you see anemia upward of 7% to 10%. As you progress through stages IV and V, it continues to go up. By the time you’re stage V, about 65%, 70% of our patients will have some form of anemia.
However, from a population standpoint, 1 thing that’s fascinating from the data is that it seems this anemia is undertreated. Based on utilization and claims data, it seems that only about 20% or 30% of anemic CKD patients will receive an ESA [erythropoietin-stimulating agent] in any given 12-month period. This is important because, as we’ve all alluded to here, this can be a quality-of-life issue. Anemia is very prevalent, and if it goes underrecognized from a health plan standpoint, it seems that these patients have a higher health care utilization as their anemia progresses, not to mention the quality-of-life issues.
Peter L. Salgo, MD: Monitoring this anemia costs money. How do you structure this? What are you willing to pay for in terms of monitoring them repeatedly in terms of their anemia?
Stanley Crittenden, MD: We tend to stick with the typical clinical practice guidelines. KDIGO [Kidney Disease: Improving Global Outcomes] is probably the most well-known guideline, and we guide our clinician partners and nephrologists to roughly mirror those guidelines. In stage III patients, most folks are getting hemoglobin checks at least once a year. Remember, we just said that stage III patients have a minority of anemia, but by the time they’re stage IV, we’re looking to hemoglobin levels usually about twice a year. By the time they’re stage V, quarterly. Of course if they’re on dialysis, it’s once a month.
Another thing we always like to see in the data is that, if they do have anemia, we like to see some further investigation to get to the root cause of that anemia. Has their iron storage been checked? Is this bleeding? Should a colonoscopy be happening? Are they having their other substrates checked like B12 and folate? We want to get a good picture of what the underlying cause of anemia is because sometimes it’s not just simply the CKD alone.
Peter L. Salgo, MD: This is a very unusual conversation I’m having with a payer. You sound very proactive. In fact, you’re willing to spend health care dollars aggressively, it sounds like, to get to the bottom of this. Is that a judgment on your part: If we can get this and find the root cause, eventually you’re going to spend less?
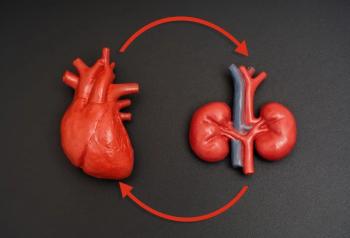
Stanley Crittenden, MD: Right. We know that health care resource utilization is increased in people with anemia of CKD, and this is also a clinical quality-of-care issue. We know that anemia in CKD is associated with some of these things that Bob alluded to: cognitive impairment, sleep disturbances, perhaps more cardiovascular complications, and perhaps even faster progression of their CKD to ESRD [end-stage renal disease]. Your direct health plan costs will be more if patients are having more quality-of-life issues—fatigue, depression—and then they will become higher health care resource utilizers.
For improved patient care, clinicians should probably know that anemia—at least it seems from claims utilization data—is probably a predictor of worse outcomes, and these are independent of the costs of the treatment of anemia. We should be focusing on these evidence-based numbers to keep folks’ hemoglobin levels at least in a decent range. This is especially true for elderly patients, who have increased risks for falls, which of course leads to hospitalization and then to increased health care resource utilization.
Peter L. Salgo, MD: If I hear you correctly, what you’re saying is that the anemia as an independent variable impacts everything and that the health care utilization in anemic patients is higher, so you’re going to make an aggressive effort to keep the hemoglobin normal.
Stanley Crittenden, MD: Correct. Normal within limits, meaning not a normal hemoglobin. Again, we want to make sure we’re staying true to our guidelines here, so normal in a CKD patient would be 10 g/dL, not 8 g/dL.
Peter L. Salgo, MD: Yeah, that’s where I was going to go. What is normal? Normal is 38 g/dL, 39 g/dL, 40 g/DL, 41 g/dL? That’s not what we’re looking at here. Let’s talk to our clinicians. Where do you look to set a hemoglobin in somebody with chronic kidney disease? Who wants to tackle that?
Robert Provenzano, MD, FACP, FASN: Let me start, and then Dan will weigh in. There’s been a lot of change over the last several years as we’ve learned more about where the proper hemoglobin level should be. There were several trials a few years back: the TREAT and CHOIR trials. They’ve shown us that high hemoglobin levels, particularly in patients who require high erythropoietin doses to reach those hemoglobin levels, had higher cardiovascular outcomes. A lot has changed.
Prior to those trials, most nephrology practices were giving iron infusions as needed and erythropoietin injections as needed, and a much higher percentage of CKD patients were having their anemia treated. It was convenient; it was done at a single visit. Since the trials suggested poorer cardiovascular outcomes, there’s a black box warning, so now nephrologists will treat anemia to avoid transfusion and, to Stanley’s point, not let the hemoglobin drop below 10 g/dL.
That has then shifted the therapies for anemia from the nephrologist’s office to a second site, typically an infusion center or an oncologist’s office. The problem with that is that there’s a disconnect from nephrology. But more important, the patients now have an additional burden to manage their hemoglobin, particularly in Detroit where many of our patients have to take buses to get to their office visits. It’s almost impossible. To Stanley’s point, the number of patients treated with CKD anemia has plummeted. Dan, I know you have your own situation in St. Louis.
Daniel W. Coyne, MD: Yeah. There’s been a big shift. Prior to 2006 and certainly 2009, nephrologists generally started treating anemia when the hemoglobin levels were in the 10s and certainly in the 9s, and the treatment was overwhelmingly to give them epoetin: Aranesp [darbepoetin alfa] or Procrit [epoetin alfa]. Secondarily, they might or might not get IV [intravenous] iron, and they would frequently get oral iron.
With the publication of some major trials showing that these increased the risk of cardiovascular events, all that has gone away. There’s a great hesitancy to treat. The average nephrologist won’t even reach for Aranesp [darbepoetin alfa] or Procrit [epoetin alfa] unless the hemoglobin is persistently in the low 9s and sometimes in the 8s, and we don’t usually treat them to much above 10. Frequently, we wave our hands and say it’s good enough when they hit the mid-9s. There has been this big pullback from using those at all: a little increase in IV iron but not as much as the data indicates should have happened.
Peter L. Salgo, MD: That’s where I was going with this. We know the cardiovascular data are getting stronger. People with higher iron stores have increased cardiovascular risk, so it’s a moving target at this point. Things are changing.
Daniel W. Coyne, MD: We have data in heart failure patients and half of those have CKD. Giving IV iron to these patients makes their heart failure better. They’re far less likely to be admitted, and their quality of life gets better. If they’re anemic, that gets better too, so they’re all tied together.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.