- Center on Health Equity and Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Interventions Needed to Increase DMT Uptake in Sickle Cell Disease
A recent study found that uptake of disease-modifying therapies (DMTs) has been low among patients with sickle cell disease, suggesting that more interventions that consider individual patient characteristics are needed to improve adoption.
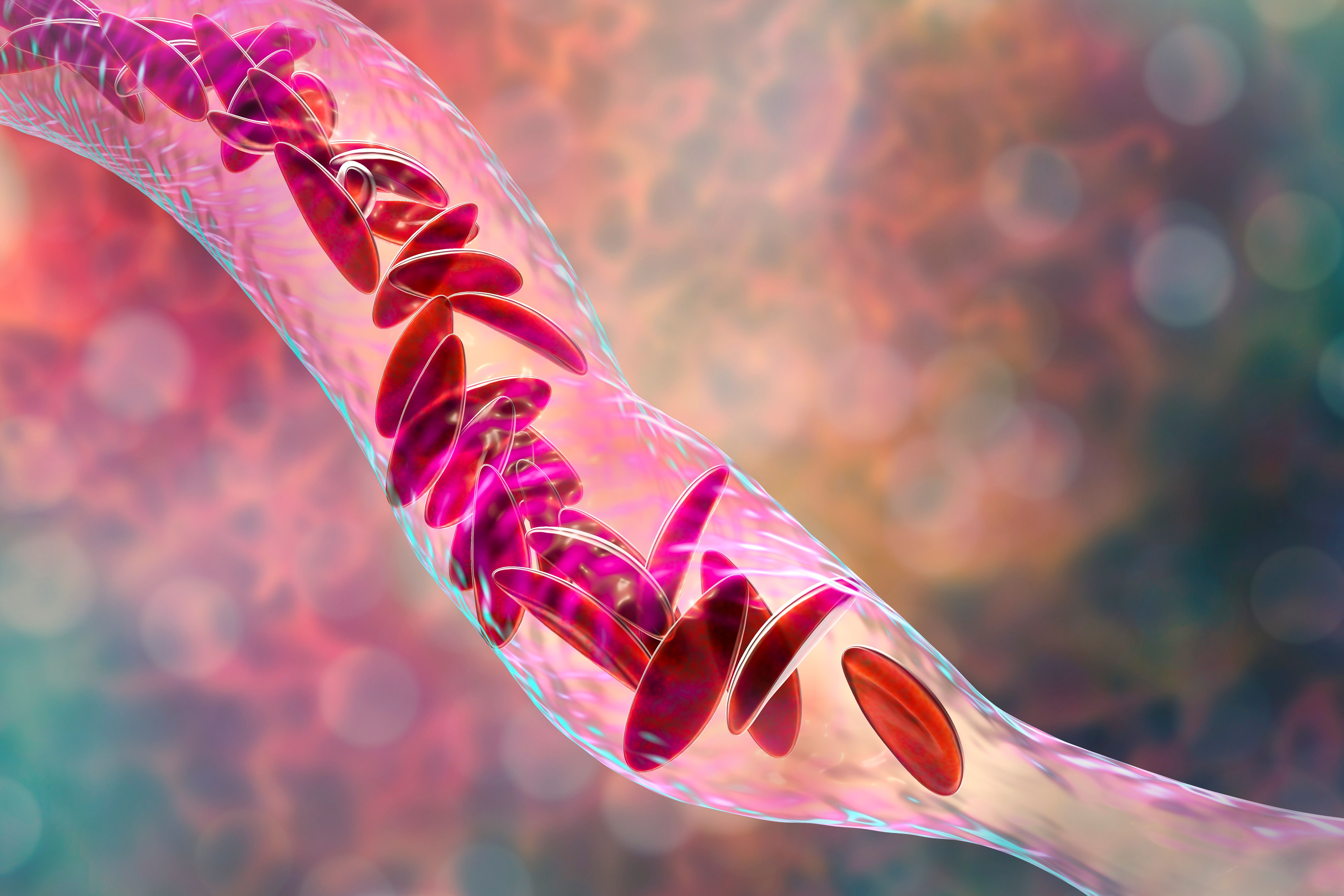
Uptake of disease-modifying therapies (DMTs) among patients with sickle cell disease (SCD) has been low between 2014 and 2021, suggesting that interventions to improve adoption need to consider individual patient characteristics, according to a recent study published in JAMA Network Open.1
Although hydroxyurea has been available to patients with SCD since the 1980s,2 its use remains low, despite it being the only pharmaceutical DMT available for use in SCD until 2017. Since then, 3 other DMTs (L-glutamine, crizanlizumab, and voxelotor) have been approved but remain underused. A previous survey revealed that less than 50% of patients with SCD reported using any DMTs within the previous month, indicating inadequate uptake.
This is the first cross-sectional study to conduct a comprehensive evaluation of DMT use since newer DMTs targeting SCD have become available.
The analysis leveraged claims data from Optum’s deidentified Clinformatics Data Mart Database from January 1, 2014, to September 30, 2021, to identify individuals with SCD. Data analysis took place from August 1, 2022, August 28, 2023. The researchers identified 2 sets of samples and applied different continuous enrollment criteria to address 2 main objectives: understanding baseline characteristics among groups using DMTs (sample A) and examining individual and overall DMT use over time (sample B). For inclusion, patients had to maintain continuous enrollment for a minimum of 6 months before and after the index date.
Overall, 5022 patients with SCD were included in sample A and 6387 were included in sample B. In sample A, 144 (2.9%) were inconsistent users of DMTs, 274 (5.5%) were incident DMT users, 892 (17.6%) were consistent users, and 3712 (73.9%) were nonusers of DMTs. In total, 41.4% (n = 2081) of the cohort was aged 18 to 45 years, and 1027 (20.5%) patients were younger than 18 years. Female patients comprised 58.3% of the cohort and the mean (SD) 6-month preindex vaso-occlusive crises (VOCs) count was 1.3 (3.1).
Users with inconsistent adherence to treatment exhibited higher prevalence rates of VOCs (mean [SD], 3.7 [4.7]), splenic complications (n = 6 of 144 [4.2%]), pulmonary complications (n = 36 of 144; 25.0%), kidney disease (n = 21 of 144; 14.6%), acute chest syndrome (n = 18 of 144; 12.5%), and health care visits (mean [SD] inpatient visits, 7.0 [10.7]) compared to other groups of users.
Nonusers of DMTs had the lowest prevalence of VOCs (mean [SD], 0.8 [2.4]), acute chest syndrome (n = 109 of 3712; 2.9%), and inpatient (mean [SD], 2.0 [6.6]) and emergency department (mean [SD], 0.7 [3.1]) visits. They also had the highest proportion of adults aged 65 years and older (n = 593 of 3712; 16.0%).
In sample B, the use of hydroxyurea moderately increased from 428 of 2188 participants (19.6%) in 2014 to 701 of 2880 (24.3%) in 2021. L-glutamine use experienced a brief increase but gradually declined throughout the study period.
In 2021, out of 2880 participants, 102 (3.5%) had at least 1 fill for crizanlizumab, and 131 (4.6%) had at least 1 fill for voxelotor. Overall DMT use increased from 19.6% in 2014 to 28.3% in 2021, driven by new treatments. However, less than 5% used newer DMTs, and nearly 75% received no DMT.
The researchers attributed the gaps in utilization to limited national awareness and funding, emphasizing the need to optimize DMT use. Barriers to usage, impact of disease severity, and initiation strategies require further exploration.
“To gain a more comprehensive understanding of DMT use, future analyses should link examinations of use over time with an exploration of the various patient-level, health system–level, and clinician-level factors or barriers that facilitate or impede DMT use. Additionally, as more research becomes available to guide the appropriate use of DMTs, it will be important to conduct further utilization studies to identify areas where intervention strategies can be deployed to improve the use of DMTs,” wrote the authors.
The study recognizes limitations, such as relying solely on prescription fill data without insight into actual medication use, lacking individual-level factors influencing eligibility for DMTs, and not including patients receiving Medicaid benefits.
The researchers concluded, “Our results underscore the importance of conducting additional research to understand and address barriers to DMT utilization. They also highlight the necessity of advocating for clinical and policy initiatives aimed at improving the development and use of DMTs within this population. Ultimately, increasing access to and use of DMTs has the potential to improve outcomes and quality of life for individuals with SCD.
Reference
1. Newman TV, Yang J, Suh K, et al. Use of disease-modifying treatments in patients with sickle cell disease. JAMA Netw Open. 2023;6(11):e2344546. doi:10.1001/jamanetworkopen.2023.44546
2. Hydroxyurea for sickle cell disease. American Society of Hematology. Accessed December 19, 2023. https://www.hematology.org/-/media/hematology/files/education/hydroxyurea-booklet.pdf
NCCN Guidelines Update Adds Momelotinib Below Ruxolitinib for High-, Low-Risk Myelofibrosis
January 23rd 2024Momelotinib was given category 2A and 2B status for patients with high- and low-risk myelofibrosis (MF) and MF with anemia. However, ruxolitinib retains a higher category of recommendation as a treatment for patients with MF.
Read More
Oncology Onward: A Conversation With Dr Shereef Elnahal, Under Secretary for Health
April 20th 2023Shereef Elnahal, MD, MBA, under secretary for health at the Veterans Health Administration (VHA), sat for a conversation with our hosts Emeline Aviki, MD, MBA, Memorial Sloan Kettering Cancer Center, and Stephen Schleicher, MD, MBA, Tennessee Oncology, that covered the cancer footprint of the VHA.
Listen
Exploring Payer Coverage Decisions Following FDA Novel Drug Approvals
May 3rd 2022On this episode of Managed Care Cast, Ari D. Panzer, BS, lead author and researcher, then at Tufts Medical Center—now at Duke University—discusses the findings from his team’s investigation into coverage decisions by health plan insurers of the 66 drugs approved by the FDA in 2018.
Listen
Exagamglogene Autotemcel Meets End Points in Severe Sickle Cell Disease, β-Thalassemia
December 7th 2023Two posters set to be presented at the 65th American Society of Hematology Annual Meeting & Exposition met their primary and secondary end points regarding exagamglogene autotemcel therapy for sickle cell disease and β-thalassemia.
Read More