HIMALAYAS Trial: Long-Term Cardiovascular Safety Data
The panel evaluates the pooled long-term cardiovascular safety data from the HIMALAYAS trial.
Transcript
Peter L. Salgo, MD: What was the pool of long-term cardiovascular safety data here?
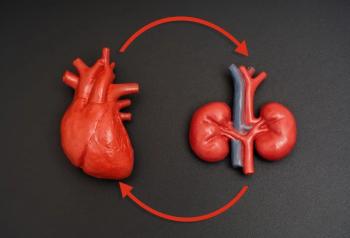
Robert Provenzano, MD, FACP, FASN: Let’s start where we all like to start. There are 2 focuses when we do these trials: does it work compared to either no therapy or to the standard therapy with the standard therapy being ESAs [erythropoietin stimulating agents]? The answer to that is absolutely: roxadustat treated the anemia, and there were no problems of efficacy compared to either the placebo in the CKD trials or to an active comparator ESA in the dialysis trials. When it comes to safety, it is exciting. What we focused on, to Dan’s earlier point, is major adverse cardiovascular events [MACEs] and then MACEs Plus, which adds to that congestive heart failure or hospitalization.
In the CKD [chronic kidney disease] population, when comparing therapy, patients treated with roxadustat to placebo, the safety signals were identical, which of course, makes sense because you’re comparing it to placebo, which is nothing. Importantly, in the dialysis population, we saw major advantages to the therapy with roxadustat. In the most vulnerable population, that is the patients with incident dialysis, let me tease this out. Those are the patients who typically crash on the dialysis, and by that, I mean that they end up in the hospital. They may have had little to no CKD management and no management of anemia. The nephrologist sees them and says, “Oh my God, we have to start emergency dialysis.” These patients are the sickest of the sick; their mortality in the first 3 to 4 months of dialysis is almost double what a prevalent patient’s mortality is. Those patients in the HIMALAYAS trial had a 30% lower MACE and a 34% lower MACE Plus safety signal. That is huge.
Peter L. Salgo, MD: I was about to say that you normally hear studies say, “We got 3% here or 10%.” Thirty percent is a lot; it’s big.
Robert Provenzano, MD, FACP, FASN: Yeah, it’s a lot.
Peter L. Salgo, MD: With a good P value, I assume.
Robert Provenzano, MD, FACP, FASN: Yes. I can’t remember the P value off the top of my head, but it was significant. Dan probably remembers it off the top of his head. When you then go to the prevalent patients, we saw a 30% MACE Plus advantage. If you’re a patient and you’re saying, “I want to do the best I can do on dialysis,” then you should look at these data. To Dan’s earlier point, patients don’t read the package insert. You’re going to want to choose something that gives a 30% advantage.
Peter L. Salgo, MD: You know what patients do read? They read Google.
Robert Provenzano, MD, FACP, FASN: Yeah, I know, I know, I know. Dan, I don’t know if I’ve left anything out because I know you were deep in these data.
Daniel W. Coyne, MD: You covered it. The main issue is that we didn’t see an increase in cardiovascular events compared to placebo in the patients not undergoing dialysis. There are some data; they’re difficult to manage because it turned out that the patients in these trials (of patients not on dialysis) were much later in their CKD than in even the TREAT trial. We were looking at people on the edge of stage 4 to stage 5 who entered these trials. They were more anemic, they had lower GFRs [glomerular filtration rates], and they were much more likely to be getting on to dialysis in the next 6 to 24 months.
The patients on placebo quickly ran into serious issues with severe anemia, and they needed either rescue therapy with ESAs or were starting on dialysis and needed to start ESA therapy, whereas the people getting their anemia treated with the roxadustat pill wound up having improvement in their anemia quickly and reductions in transfusions, in addition to not having an increase in cardiovascular events.
Peter L. Salgo, MD: You said something just there that is important. I want to make sure everybody heard this: it’s a pill.
Daniel W. Coyne, MD: It’s a little pill.
Peter L. Salgo, MD: It’s not an injection, and it doesn’t have to be refrigerated, right?
Daniel W. Coyne, MD: Right.
Peter L. Salgo, MD: You take it home; you don’t have to come
Daniel W. Coyne, MD: Yes. It seems to enhance their iron absorption. The beauty of the physiology is that every time they take this pill, the body has a brief stimulation in production of epoetin that then goes back down to baseline, and a bit of enhancement of iron absorption and iron released from the body. That anemia of chronic disease is iron locked up in your macrophages. This helps release that, so it treats this anemia of chronic disease 2 different ways, not just through pharmacologic epoetin.
Peter L. Salgo, MD: That’s fascinating.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.