Future Management of Anemia in CKD
Closing thoughts on the future landscape of treating patients with anemia in CKD.
Transcript
Peter L. Salgo, MD: With all of this, what do you see as the future of treating anemia and CKD [chronic kidney disease] going forward?
Robert Provenzano, MD, FACP, FASN: Well.
Peter L. Salgo, MD: It wasn’t that funny.
Robert Provenzano, MD, FACP, FASN: When I look at CKD, I tell this story. When I was an intern, and you came into the ER [emergency room] with a heart attack, I’d always ask the fellows, “Do you know what we did?” They would look at each other, and I said, “We did nothing. We maybe put some nitroglycerin paste on him and wished him well for the night and hope they lived.” We didn’t have catheterization labs. Today, you’re in the catheterization lab within the first hour, and you get a cardiac catheterization. You don’t have an MI [myocardial infarction], and you go home. They look at me, mortified.
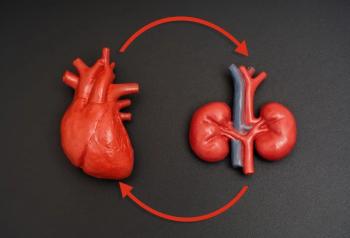
My view of chronic kidney disease is this: my hope is that we will have therapies, maybe roxadustat and the HIF-PHIs [hypoxia-inducible factor prolyl hydroxylase enzyme inhibitors] are going to be part of that, where you don’t even go into kidney failure. If you end up in kidney failure, there’s something significantly missing in your identification in therapy. When it comes to management of anemia, I see that as a critical piece of the puzzle to delay the symptoms and/or progression, in addition to now, how as we know SGLT2 [sodium glucose cotransporter-2] inhibitors show positive outcomes in delay. Each of these are a piece of a puzzle, to Stanley’s point, putting it all together and focusing on individual patient care.
Peter L. Salgo, MD: This is an exciting moment, it sounds like to me. Before we leave, what I want to do is go around to each of you and get some pithy thought, real pith here. Maybe you could give me 1 final thought to sum up a critical point you’d like to leave with our viewers. Why don’t we start with Dr Crittenden?
Stanley Crittenden, MD: My final point would be that we should continue to consider the total patient experience and total patient care, not focused on 1 thing in a silo. Consider their anemia, how it relates to their CKD progression, and how it relates to their diabetes control because that’s ultimately what we’re striving for, which is truly an improved patient outcome.
Peter L. Salgo, MD: Dr Coyne, you’re next.
Daniel W. Coyne, MD: Be pithy. I would say that I hope these drugs make anemia much less a focus for nephrologists. There’s a lot of important things that we need to take care of in the cardiovascular health of our patients, and I’d like to just give them a pill and know that their anemia is taken care of, so I can just move on to more important things.
Peter L. Salgo, MD: Dr Provenzano, you’ve got the last word.
Robert Provenzano, MD, FACP, FASN: Gosh almighty, that’s the first time I’ve ever had the last word. My comment would be that we are moving from a 20th century pharmacologic management of anemia to a 21st century physiologic management of anemia, which, to me, is incredibly exciting.
Peter L. Salgo, MD: I want to thank all of you for joining us today. This has been fascinating for me as a non-nephrologist. From what I’m hearing, along with lots of other disease states and lots of other specialties, this is a new age in the way we approach disease and its management, and it’s great to be a doctor. I’m excited about this. I want to thank you for being here, I want to thank our viewers for joining us, and I hope everybody found this AJMC panel discussion useful and interesting. I’m Dr Peter Salgo, and I’ll see everybody next time.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.