- October 2021
- Volume 27
- Issue 7
Conversations on CAR T: UAB’s Mehta Discusses Opportunities and Challenges
This summer, Evidence-Based Oncology™ (EBO) conducted in-depth interviews with experts on current research and practice in chimeric antigen receptor (CAR) T-cell therapy, including opportunities and challenges in academic and community settings. This interview is with Amitkumar Mehta, MD, director of the Lymphoma Program and Immune Effector Cell/CAR T Program and an associate professor at the University of Alabama at Birmingham (UAB). Mehta discussed a review paper he coauthored that appeared in Annals of Translational Medicine,1 which raised the issue of financial toxicity that many patients face. He also discussed the development of markers to gauge who can safely receive outpatient CAR T-cell therapy and why he advises his patients to keep wearing their masks.
The interview has been edited for length and clarity.
EBO: Let’s discuss the review paper on CAR T-cell therapy published in June. One idea you present is the concept of universal CARs. Can you elaborate?
MEHTA: If you look at CAR T treatment, it is one of the best for relapsed diffuse large B-cell lymphoma (DLBCL)—it has definitely changed the treatment paradigm. If patients have the first
relapse—whether [they are] transplant eligible or not or…high-dose chemotherapy eligible or not, based on their comorbidities and performance status—once they cross the second-line therapy
and the third-line therapy everybody looks at the care team: are all patients able to go to CAR T? The answer is no. There are a variety of reasons, including the distance from the academic center, because most CAR T treatments are offered at academic centers or large community-based practices. So if the doctor’s practice is in rural Alabama, the patient must travel all the way to the academic center to get CAR T therapy. That’s one factor.
Another is insurance—it’s a big challenge. The third is that this disease is aggressive; patients progress very fast. We have very limited time for factors like insurance approval and for doing some of the testing before pursuing CAR T, or for the case-based agreement that the institutions have to do with the insurance company. These are all limiting factors for offering this life-saving treatment for patients.
So how can we make it universal? That was my concept––whether we can bring it to the community centers, where we can have a concept of a formal partnership in which academia can create teams that…offer treatment locally or closest to the patient, or whether we can have off-the-shelf CAR T, where the patients don’t have to wait for the preparation time, which ranges from 2 weeks to 6 weeks depending on which product you’re using.
Also, off-the-shelf CAR T reduces the preparation time as well as availability. So, if I…have a patient who has to go for a treatment, I say, “Well, I’m going to prescribe this, which will be available next week,” compared to 6 weeks from now. Those factors will make this treatment universal.
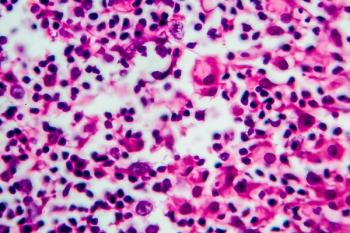
Other subtle factors that come in are to do with biomarkers, such as a biomarker-driven prediction as to whether this patient will develop toxicities like cytokine release syndrome or neurotoxicity,
or whether this patient will respond or not. That way we can predict the outcome of not only the toxicity but also the efficacy of treatment.
EBO: How close are we to getting allogenic or “off the shelf” treatment? It has been discussed for a while now. Are we getting closer?
MEHTA: At the American Society of Clinical Oncology there were a few phase 1 studies published, and they are being expanded. At the [December American Society of Hematology] meeting we’ll have further updates. There are a few therapies—I would put them in the cellular therapy category— and one is definitely CAR T. A second is CAR-NK (natural killer), where we are transfecting these NK cells. The third emerging therapy is activated NK cells…and they are being combined with other CD-20– or CD-19–directed therapies to see how the outcomes are. The activated NK and T-cell therapies have been used in Epstein-Barr virus (EBV)-driven lymphomas and EBV-driven malignancies before. So it’s not just CAR T, but we are also looking at other ways to expand the cellular therapy offering to lymphoma patients. It will be very exciting in the next 3 to 5 years when we might have some of this approved.
These treatments do come with adverse effects, so if you have allogenic cellular therapy—just like allogenic transplant—we may have to look at the additional toxicities in terms of graft-vs-host disease. Apart from the toxicities that we see with autologous CAR T cells, where the patient’s T cells are transfected…, there could be an added adverse effect of graft-vs-host disease, which may have a longer or shorter duration.
EBO: You have discussed the challenges you’re having with finding biomarkers to identify the patients who are at risk for toxic effects. How far away are we from having really good biomarkers so we can stratify patients?
MEHTA: We still don’t have any biomarkers, but there are some indirect indicators that we can discuss. One of them is how bulky the disease is, whether the patient’s lactate dehydrogenase is
elevated right from the beginning or whether the patient has elevated ferritin or C-reactive protein levels. That can tell us that these patients may develop more cytokine release syndrome or the neurotoxicity syndrome. Hopefully, in a couple of years, we might have a predictive index to tell us “this patient could develop cytokine release syndrome” or “the patient will have higher chances compared with other patients.”
Why is this important? Of course, it is very important for the safety of the patients. But another aspect is very key, which many of the payers might be interested in, especially at institutions such as mine where we have rolled out an outpatient CAR T program. We want to make sure that those who are outpatients are at low risk of developing cytokine release syndrome and the neurotoxicity. If we can manage them as outpatients, the patient doesn’t have to go in the hospital for 7 to 10 days.
Why is it critical at this point? Because of the COVID-19 pandemic. As you know, the Delta variant cases are rapidly rising; hospital beds are full with those patients. Therefore if I have to plan for a CAR T patient, and if I say I need 7 to 10 days for an inpatient bed, the hospital administration will look at me and say, “You know, it may not be possible.”
So if we can we avoid those kinds of challenges, based on predictive markers that show a patient is low risk, we can treat a patient as an outpatient instead of admitting him. The other factor from a payer perspective is whether there is a change in the incentive model. With outpatient regimens and treatments they’re paid differently compared to inpatient, and most of the inpatient regimens, as you know, are way more expensive for both the hospital and the payer. If you have a predictive marker and an index that can say this patient is low risk, and we can treat them on an outpatient basis, there may be a huge difference in finances compared with a patient who is treated as an inpatient. So those factors are very critical. And I am very positive that based on the markers we’re looking at we will come up with some type of index in the next couple of years.
EBO: Speaking of COVID-19, how are you handling patients with DLBCL and vaccination? Have you
developed a set of protocols in terms of timing, vaccination, and treatment?
MEHTA: For most of my patients on therapy, I ask them to get vaccinated. If you look at the recent
CDC recommendations, they’re suggesting a booster for immunocompromised patients. If I’m
starting any patient on new treatment, I’m highly recommending that they get the vaccine before they start the treatment. They’re immunocompetent right now, so they can impart an immune response. That way they are protected. As with other immunocompetent people, if they’re on the therapy and they have not received the vaccine, I asked them to get vaccinated at the earliest opportunity. And that can happen during the time where their counts are coming up so that they can get the vaccine. But I do know that if they’re on the treatment, or within a few months after completion of treatment, they may not have the immune response needed. So there is a time that I suggest they get the booster when they finish the therapy. My arbitrary timeline is around 4 to 6 months. Once they finish the chemotherapy, 4 to 6 months out, I ask them to get a booster dose or the vaccine.
Many times I am asked whether that decision is based on the antibody titers. We don’t have any data yet. What is the cutoff ? I don’t even know whether there is a certified test available on which we can base a decision that says, “Your titer level is this high, that’s why you don’t need a booster,” or “This is low; you need a booster.” We don’t have that kind of flowchart yet from the CDC. But I hope we get guidance in the future.
EBO: I was going to ask whether you test for antibodies but it sounds as though it’s all still too new.
We’ll just have to wait.
MEHTA: So far, the information we have is that the cancer patient undergoing treatment for patients with lymphoma and chronic lymphocytic leukemia (CLL), either on or off treatment, are not importing the immune response like immunocompetent people. So that’s [one reason] that I still ask my patients to practice masking and social distancing. Because even though they are vaccinated––and either they recently finished treatment or they are on treatment––CLL itself makes you immunocompromised. You should not be that confident that [you say,] “Yes, I’ve got a vaccine and I can take off my mask.” For their protection, I highly recommend that they put on a mask, especially in crowded places like churches or malls.
Reference
1. Narkhede M, Mehta A, Ansell SM, Goyal G. CAR T-cell therapy in mature lymphoid malignancies: clinical opportunities and challenges. Ann Transl Med. 2021;9(12):1036. doi:10.21037/atm-20-5546
Articles in this issue
over 4 years ago
From the Editor-in-Chief: The Way Upover 4 years ago
Building a Patient-Centered Cancer Center From the Ground Upover 4 years ago
The Promise of Liquid Biopsies for Cancer DiagnosisNewsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.