Contributor: How Payers Can Be Effective in New Value-Based Models for CKD
The author discusses how value-based payment models in chronic kidney disease can improve total cost and quality of care for patienst with chronic kidney disease (CKD).
Value-based care has been replacing the traditional fee-for-service model that has been the dominant health care payment model in the United States. The
Value-based care models and population health are essential to improving health and reducing health care costs. Change comes in many forms and the healthcare landscape has many examples of joint ventures, partnerships, and collaborations. Alliances can position payers and health care providers to drive value-based care by leveraging their strengths.
A recent example of this was the Humana and Fresenius Medical Care North America (FMCNA) announcement of
The driving force behind this expanded collaboration is due in part to the 21st Century Cures Act, which allows patients with ESRD to enroll in Medicare Advantage Plans
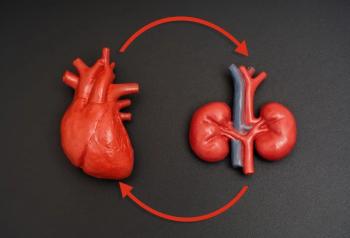
Kidney disease ranks as the ninth leading cause of death in America. Over 37 million people are suffering from CKD and more than 726,000 have ESRD, with 100,000 patients waiting to receive a kidney transplant, according to HHS. Approximately 1 in every 5 dollars in traditional Medicare, $114 billion per year, is spent on patients with kidney disease. Twenty percent of the 100,000 patients who begin dialysis for ESRD each year will die within a year.
To reduce the development of ESRD, CMS, through the Innovation Center,
The ETC Model adjusts certain Medicare payments to ESRD facilities and clinicians managing patients with ESRD through upward or downward payment adjustments based on their home and transplant rates to increase use of home dialysis and rates of kidney transplants. Specifically, CMS will positively adjust certain Medicare payments to the participating ESRD facilities and clinicians for the first 3 years of the model for home dialysis and dialysis-related services. The ESRD facilities and clinicians are randomly selected based on geographic location to account for approximately 50% of adult Medicare patients with ESRD. The ETC Model will impact approximately 30% of kidney care providers beginning January 2021, and is estimated to save $23 million over 66 months.
The 4 optional Innovation Center models, KCF, CKCC Graduated, CKCC Professional, and CKCC Global, are designed to help healthcare providers reduce the cost and improve the quality of care for patients with late-stage CKD and ESRD. The models are also designed to delay the need for dialysis and encourage kidney transplantation.
In the KCF Model, nephrology practices will receive adjusted fixed payment on a per-patient basis for managing the care of patients with late-stage CKD and ESRD. Payments are adjusted based on health outcomes and utilization compared with the practice’s own experience and national standards, as well as performance on quality measures. Each patient who receives a kidney transplant will receive a bonus based on the transplant remaining healthy, for up to 3 years after surgery.
The CKCC Models include capitated payments like the KCF Model, but the Kidney Contracting Entities, made up of nephrologists, transplant providers, and other healthcare providers including dialysis facilities, will have accountability for the total cost and quality of care for their patients. These models include both upside and downside risk components for the entities.
In alignment with the Advancing American Kidney Health Initiative goals and the objectives of the Innovation Center Models, the Humana-Fresenius expanded collaboration also goes into effect on January 1, 2021, and will include 3 main components: expansion of care coordination services to an additional 39 states from the current 3, transition care units for people recently diagnosed with kidney failure, and a value-based renal care agreement.
The value-based component is stated to be aligned with the objectives of CMS’s ETC Model, by encouraging increased adoption of home dialysis and improved access to kidney transplants. The payment model includes in-center and home dialysis services, the Transitional Care Units, and CKD care coordination services, basing compensation on meeting certain agreed on quality improvement and patient outcome goals, and reducing overall costs to the system.
By linking the providers and payers in models that are aligned with improving patient outcomes and reducing costs to the health care system, patients will also benefit through improved outcomes. These 2 examples demonstrate models that payers can leverage to work with health care providers in partnerships to share downside risks associated with poor health and the upside benefits accompanying good health.
Reducing the cost of health care while improving it may seem counterintuitive, but that is only because the traditional fee-for-service system is designed to promote volume not value. Value-based care will continue in the future as providers and payers expect to increase collaboration on patient engagement, population health management, and access to care. Through collaboration with public and private payers and healthcare providers, a new value-based model of care focusing on outcomes and reducing cost can provide a healthy, sustainable future for our healthcare system.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.