Anemia in CKD: CHOIR and TREAT Trials
A review of the CHOIR and TREAT trials that established caution around target hemoglobin levels with ESAs in patients with anemia in CKD.
Transcript
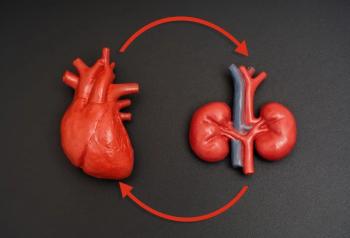
Peter L. Salgo, MD: Let me take a different tack here. We have 2 silos: one is chronic kidney disease [CKD] and the other is end-stage renal disease. Is the treatment of anemia different for each of those silos?
Daniel W. Coyne, MD: For patients undergoing dialysis, virtually everybody gets treated. In a given year, almost everybody will get some doses of epoetin, and in a given month, 90% of them are getting epoetin or a similar product, even IV [intravenous] iron. If they’re a patient undergoing hemodialysis, over the course of a year, virtually everyone gets iron in any given quarter. About 70% to 80% of them are getting iron. Very few of them avoid the need for this, so there is not much discussion and not much variation in how we treat. What we’ve talked about is CKD, and that’s dramatically different.
Peter L. Salgo, MD: Alright. We had some trials, and you alluded to the risks of ESAs [erythropoietin- stimulating agents]. The trials I know that come to mind are CHOIR, and another one is TREAT. What do they show?
Daniel W. Coyne, MD: The CHOIR trial was published in 2006. It took CKD 3 and 4 patients who were anemic and randomized them to 1 of 2 doses of epoetin, 1 being a dose adjustment to get the hemoglobin to about 11.3 g/dL and the other to 13.5 g/dL. The theory was that raising the hemoglobin to normal would reduce cardiovascular events and death, so that was the primary outcome of the study. As [Marc] Pfeffer [MD, PhD], who did the subsequent TREAT trial, pointed out, in studies like CHOIR where both arms get the drug, the drug always wins. The drug in this case won, but it was the lower hemoglobin that had fewer cardiovascular events and deaths. This was the first major nondialysis study to show significant harm from use of these drugs, and it was a wake-up call to the nephrology community.
Three years later, the TREAT trial was published. TREAT was a placebo-controlled trial as I mentioned before, and they did a lot of things to minimize cardiovascular risk: very slow increases in the darbepoetin dose. As long as the hemoglobin was going up, you didn’t get a dose increase. The thought was that this would minimize cardiovascular risk, and maybe it did, but the point was that it was supposed to reduce cardiovascular risk, and there was no reduction in cardiovascular risk or death. In fact, it doubled stroke and significantly increased thrombotic events. It did have a small effect on transfusions, but you needed to treat 10 people to avoid 1 transfusion. That’s a heck of a lot of money to avoid a transfusion.
Peter L. Salgo, MD: Was the theory there that this was a rheologic phenomenon? That the blood was thicker, it clotted more easily, it flowed more slowly, and it was giving you more strokes?
Daniel W. Coyne, MD: We’re not able to entirely tease that out. The people with increased cardiovascular events paradoxically appeared to be the people who didn’t respond to the drug, but they then, therefore, get exposed to higher doses.
Peter L. Salgo, MD: I see. It might be a direct effect of the drug.
Daniel W. Coyne, MD: At the end of the day, the way to avoid the high doses is to avoid the high hemoglobin target, and that’s where we moved because we don’t know which is the driver there.
Peter L. Salgo, MD: Is that what you’re doing here? In order to prevent the adverse effects of these drugs, Dr Provenzano, maybe you’re just not going to push them as hard? What other measures do you take in clinical practice?
Robert Provenzano, MD, FACP, FASN: Dan alluded to the answer. We found in these trials that the patients who required higher ESA doses had poorer cardiovascular outcomes. That gets to the state of inflammation. There are a couple of important things: you want to avoid high doses if you’re going to use an ESA, and if your patient is resistant to the ESA, then you don’t want to continue to expose them to higher doses. That’s my view of it, but you then get into the details of who is at higher risk. Again, it’s the individual care. If the patient has had strokes before and if they’ve had head and neck cancer before, then there’s a lot of additional risks, and that’s up to the individual nephrologist to sort through.
Peter L. Salgo, MD: Give me a bullet point here. When do you pull the trigger and transfuse?
Daniel W. Coyne, MD: I follow the AABB [The American Association of Blood Banks] guidelines, which is that I don’t transfuse unless the hemoglobin level is less than 7.0 g/dL, or if they have cardiovascular disease, then it’s less than 8.0 g/dL. If they’re a stable outpatient, they’re less than 8.0 g/dL, and they’re a candidate for ESAs or IV iron, I’m going to try to use that. Acuity influences it, too.
Robert Provenzano, MD, FACP, FASN: That’s where I was going to go. I’m definitely affected by acuity. If somebody has dropped from 11.0 g/dL down to 7.0 g/dL, I’m going to be fairly anxious, and if I think I need time to figure out what’s going on, I’ll be more likely to transfuse.
Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.