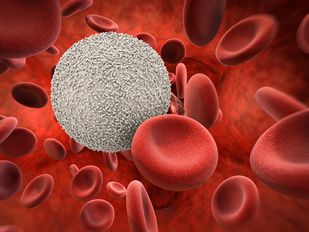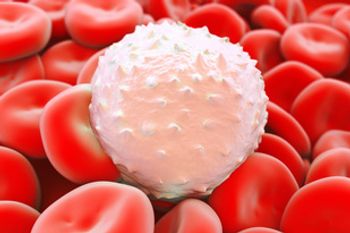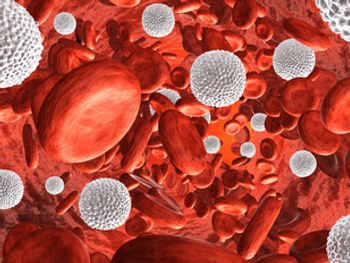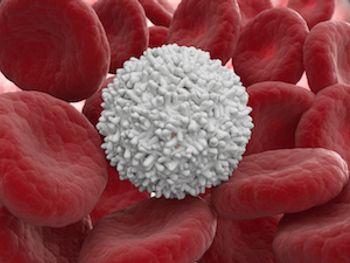
Cytarabine, aclarubicin, and granulocyte colony-stimulating factor (CAG) generates a positive effect for patients with acute myeloid leukemia (AML) by decreasing the number of immunosuppressive cell types and their associated cytokines, while also downregulating SDF-1α levels