- April 2023
- Volume 29
- Issue 4
- Pages: SP290-SP291
ACC 2023 Coverage: Topics in Cardio-oncology
Coverage from the American College of Cardiology Scientific Session Together With World Congress of Cardiology, held March 4-6, 2023, in New Orleans, Louisiana.
Patients Taking Statins Alongside Anthracyclines for Lymphoma Had Less Heart Dysfunction, Study Shows
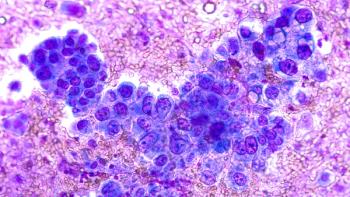
Patients treated with anthracyclines for lymphoma who took the cholesterol-lowering drug atorvastatin for 12 months showed less evidence of cardiac dysfunction, according to findings of a study presented March 4, 2023, at the 72nd American College of Cardiology (ACC) Scientific Session Together With the World Congress of Cardiology in New Orleans, Louisiana.1
The randomized trial, “Statins TO Prevent the Cardiotoxicity from Anthracyclines,” or STOP-CA (NCT02943590), enrolled 300 patients with lymphoma who were treated with anthracyclines at a median dose of 300 mg/m2. Half the patients received 40 mg of atorvastatin and half received placebo daily, starting before their first dose of anthracycline chemotherapy and continuing for a year.
Although newer treatments such as targeted therapy and immunotherapy are revolutionizing cancer care, first-line treatment with chemotherapy remains standard in many settings, including for lymphoma. According to the Leukemia & Lymphoma Society, more than 90,000 individuals will receive a diagnosis of some form of lymphoma in the United States each year.2 Study authors for STOP-CA said 1 million patients are treated with anthracyclines each year.1
In fact, the improved survival rates of patients with lymphoma have increased concerns about the cardiotoxic effects of anthracyclines, as more physicians and patients worry that the greater health risk may come from the effects of the first line of cancer treatment. As co–principal investigator Tomas G. Neilan, MD, MPH, director of the Cardio-Oncology Program at Massachusetts General Hospital in Boston, explained during the late-breaking session, “Depending on the study population, and the length of follow-up, there is a 10- to 15-fold increased risk of heart failure with anthracyclines.”
Why Atorvastatin?
Statins have been used for more than 30 years to reduce low-density lipoprotein (LDL) cholesterol, through inhibition of hydroxymethylglutaryl-coenzyme A reductase. However, as explained by Heiston and Hundley last year,3 reductions in LDL cholesterol do not fully explain all the cardiovascular benefits of statins. They write that statins have multiple cardioprotective effects and “have been shown to reduce LV [left ventricular] dysfunction in those with heart failure.” Statins’ possible role in long-term cardiac remodeling has been linked to reduced vascular inflammation and endothelial dysfunction. Heiston and Hundley offer a review of evidence of statins’ potential cardioprotective and possible anticancer effects, although much of the evidence involves observational studies with patients who were already taking statins and had diabetes or cardiovascular disease.3
By contrast, STOP-CA, funded by the National Institutes of Health, excluded patients who were taking statins or for whom statin use was indicated based on clinical guidelines.
Results for STOP-CA
The primary outcome was the proportion of patients who had a decline in the LV ejection fraction (LVEF) of at least 10% to less than 55%. The secondary outcome was the proportion of patients who had a decline in LVEF of at least 5% to less than 55%. Results were as follows:
- At baseline, LVEF across the entire cohort was 63% ± 4.6%.
- At 12 months, across the entire cohort, LVEF was 59% ± 5.9%.
- At 12 months, across the entire cohort, 46 patients (15%) had a decline in LVEF of at least 10% from prior to chemotherapy, to a final value of less than 55%.
- Adherence to atorvastatin was greater than 90%.
- Median age of patients was 52 years; 47% were women.
For the primary end point:
- The incidence at 12 months was 9% in the atorvastatin group and 22% in the placebo group (P = .002).
- The odds of a decline of at least 10% in LVEF to a final value of less than 55% after anthracyclines was almost 3 times greater for those taking placebo (OR, 2.9; 95% CI, 1.4-6.4).
For the secondary end point:
- At 12 months, 64 participants (21%) in the entire cohort had a decline in LVEF of at least 5% from prior to chemotherapy to a final value of less than 55%.
- The incidence of this secondary end point was 13% in the atorvastatin group and 29% in the placebo group (P = .001).
Among the exploratory end points:
- In both the atorvastatin and placebo groups, the average pretreatment LVEF was 63%.
- At 12 months, the LVEF for the atorvastatin group was 59%, for a mean decrease of 4%.
- For the placebo group, the average LVEF at 12 months was 57%, for a mean decrease of 5%.
- There were 11 heart failure events with no difference in the incidence of heart failure between study groups (P = .77).
Impact of Findings
“We believe that patients with lymphoma who are treated with anthracyclines and are at high risk of cardiac dysfunction and heart failure would benefit from statin therapy,” said co–principal investigator Marielle Scherrer-Crosbie, MD, PhD, professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia, who discussed the results at a news conference. “I think it’s an impactful study that will lead to more prescription of statins in patients.”
Sherrer-Crosbie said there were no safety concerns in the study; there were no differences between the 2 arms in muscle pain, myositis, or elevated liver enzymes. Neilan said that although the study did a good job of enrolling women, the trial did not have a racially or ethnically diverse enrollment, and this was a limitation.
Commenter Anita Deswal, MD, MPH, MBBS, of The University of Texas MD Anderson Cancer Center, Houston, and chair of the ACC Cardio-Oncology Section, discussed the fact that the trial measured changes in LVEF, not actual heart failure. This is not so simple, she said, and the trial team should be commended for achieving such a high level of medication adherence among patients being treated for cancer.
“While it’s easy to say they should have just looked at heart failure, we recognize the issue of getting 300 patients enrolled,” Deswal said. It is possible that as patients are followed over a longer period, more patients in the placebo arm will have heart failure.
References
1. Neilan TG, Silva TQ, Onoue T, et al. The STOP-CA Trial: Statins TO Prevent the Cardiotoxicity associated with Anthracyclines. Presented at: The 72nd American College of Cardiology Scientific Session Together With the World College of Cardiology; March 4-6, 2023; New Orleans, LA. Abstract 23-LBCT-19421-ACC.
2. Facts and statistics overview. Leukemia & Lymphoma Society. Accessed March 11, 2023. http://bit.ly/424fuHz
3. Heiston EM, Hundley WG. Statins for cardiac and vascular protection during and after cancer therapy. Curr Oncol Rep. 2022;24(5):555-561. doi:10.1007/s11912-022-01212-4
Cardio-oncology Abstracts Examine Disparities in Care, a Complex Case
Cardio-oncology is developing as an important subspecialty, for reasons both good and unfortunate. On the plus side, improved cancer survival rates mean patients are living longer, so care teams must consider the effects of prior treatments on the heart.1 On the downside, scientists are working to understand how rising obesity rates affect the development of cancer alongside associated cardiovascular risk.2 These conditions must be taken into account as regimens are prescribed. Abstracts presented at the 72nd American College of Cardiology (ACC) Scientific Session Together With the World Congress of Cardiology, held March 4 through 6, 2023, in New Orleans, Louisiana, covered many of these issues.
Comparing Cardio-oncology Data Among Teenagers vs Adults
Investigators from The University of Texas MD Anderson Cancer Center, located in Houston, used a payer database to conduct the first nationally representative, multiyear analysis of how many teenagers develop cancer along with cardiac conditions, and how their outcomes, costs, and disparities compare with adult groups.3
The MD Anderson team used the largest payer inpatient data set in the United States, the National Inpatient Sample, along with Machine Learning-augmented Propensity Score adjusted multivariable regression (ML-PSr). The propensity score was modified for the likelihood of disease.
Investigators defined cardio-oncology as active cancer and at least 1 concurrent cardiac condition, including peripheral artery disease, coronary artery disease, heart failure, cardiomyopathy, and arrhythmia.
The data set included 90,869,382 adult hospitalizations from 2016 through 2018; of these, 1,207,170 were teenagers. Among this group:
Among the teenagers, 24,840 had active cancer.
- 6045 (0.50%) had cardiac conditions.
- 405 (0.03%) had concurrent cardio-oncology conditions.
Among cardio-oncology teenagers, common primary malignancies were leukemia (44.44%), bone/connective tissue malignancy (29.63%), non-Hodgkin lymphoma (11.11%), and head/neck cancer (7.41%).
Compared with adults, teenagers with a cardio-oncology condition had “comparable likelihood” of receiving some procedures, including left heart catheterization (3.70% for teenagers vs 5.18% for adults, P = .729) and peripheral angiogram (0.00% for teenagers vs 0.56% for adults, P = .697).
However, teenagers were significantly more likely than adults to receive an implantable cardioverter defibrillator (ICD; 3.70% vs 0.20%; P < .001). In ML-PSr fully adjusting for clinical severity and confounders, teenagers were significantly more likely to die while hospitalized inpatient than adults (OR, 1.48; P < .001) and have increased costs ($4046.89; P < .001). However, teenagers specifically with cardio-oncology conditions had comparable mortality as adults, and in this study they did not report any significant disparities by sex, race, income, insurance, urban density, or region relative to adults.
Black Patients More Likely To Be Hospitalized for Acute HF
Investigators from Louisiana State University Health Sciences Center, New Orleans, presented data examining hospitalization rates by race for patients who have cardiac dysfunction related to cancer treatment. Although prior studies have shown Black patients are more likely to develop cancer treatment–related cardiac dysfunction, these data were limited to prevalence and outcomes of acute heart failure.4
The team used the National Inpatient Sample from 2016 through 2019 and identified hospitalizations with a diagnosis of cancer treatment–related cardiac dysfunction using International Classification of Diseases, Tenth Revision codes along with χ2 test and logistic regression to identify the association.
Over the period studied, 18,515 hospitalizations were identified involving cancer treatment–related cardiac dysfunction, including 6050 (32.7%) involving a diagnosis of acute heart failure. Being a Black adult was independently associated with acute heart failure (adjusted OR, 1.24; 95% CI, 1.15-1.35; P < .001), after adjusting for age, race, and baseline cardiovascular risk. However, the investigators found that being a Black adult was not an independent predictor of in-hospital mortality in patients with acute heart failure (aOR, 0.98; 95% CI, 0.75-1.27, P = .89).
Baseline data provided with the abstract showed that Black patients with cancer (n = 3535, vs n = 14,980, rest of the population) were more likely to be obese (14.4% vs 9.5%), more likely to have hypertension (67.8% vs 55.5%), and more likely to have diabetes (28.6% vs 21.6%). The Black patient population in the study was 70% female, compared with the rest of the population, which was 58.2% female. The Black patient group was slightly more likely to have renal failure, 26.9% vs 22.5%, respectively. The Black patient group was much less likely to have hypothyroidism, 1.5% vs 17.1%, respectively.
According to the investigators, “These findings might suggest underlying inequities in screening and preventive cardio-oncology care and highlight the unmet need to address the social determinants of health in patients with cancer and comorbid cardiovascular disease.”
Case Study Describes Cardio-oncologic Emergency
Authors from The Mount Sinai Hospital, New York, New York, describe a rare case of “Triple M” syndrome, in which the combination of myocarditis, myositis, and myasthenia gravis develops as a complication in patients receiving immune checkpoint inhibitors (ICIs). The syndrome is associated with increased morbidity and mortality.5 According to the authors, first-line therapies for myocarditis-myositis may aggravate myasthenia gravis crisis. In this case, the patient’s immune-related toxicities escalated, ejection fraction dropped, and the patient died.
In the case presented at ACC, a man aged 74 years with a history of locally advanced esophageal adenocarcinoma was treated with neoadjuvant FOLFOX (folinic acid, fluorouracil, and oxaliplatin), followed by nivolumab. He developed fatigue and dyspnea; then, 4 days after his second cycle of nivolumab, he experienced acute bilateral ptosis, or droopy eyelids; fatigable diplopia (double vision); and dysphagia, or discomfort in swallowing. His troponin I was 4.62 ng/mL. An electrocardiogram showed normal sinus rhythm, new left anterior fascicular block, and premature ventricular complexes. His creatinine phosphate kinase level was 1122 U/L. An initial echocardiogram showed ejection fraction of 52%.
As described by the authors, “The patient’s presentation was consistent with multiple moderate-grade ICI toxicities (ie, Triple M). He was initially started on methylprednisolone at 1 mg/kg, instead of pulse dose, due to concern for acutely worsening myasthenia gravis (MG). Plasma exchange (PLEX) was also started for myasthenia rather than IVIG [intravenous immunoglobulin] due to his tenuous cardiac status and concern for volume overload.”
Nonetheless, the patient developed tamponade, or pressure on the heart due to fluid build-up, which required pericardiocentesis and a transvenous pacemaker. PLEX was held and methylprednisolone was increased to 1000 mg/d. MG worsened, “requiring intubation and 6 additional PLEX sessions.
Repeat echocardiogram showed an ejection fraction of 25% with global hypokinesis and repeat troponin of 12.97 ng/mL. Mycophenolate mofetil was promptly added for his worsening immune-mediated toxicities.”
“The patient eventually proceeded with comfort care, and he passed away peacefully per his wishes,” the authors wrote.
The authors concluded, “Our goal is to educate clinicians on the spectrum of ICI toxicities and the nuances in treatment decisions. Such conditions are a cardio-oncology emergency and should be recognized by clinicians as soon as possible.”
References
1. Shi S, Lv J, Chai R, et al. Opportunities and challenges in cardio-oncology: a bibliometric analysis from 2010 to 2022. Curr Prob Cardiol. Published online April 29, 2022. doi:10.1016/j.cpcardiol.2022.101227
2. Reding KW, Simon MS, Cheng RK. Toward a more precise understanding of obesity and cancer and cardiovascular disease risk. JACC CardioOncol. 2022;4(1):82-84. doi:10.1016/j.jaccao.2022.02.004
3. Iliescu C, Alexandrescu S, Monlezun D, et al. Cardio-oncology prevalence, mortality, cost, and disparities for teenagers: machine learning analysis of 1.27 million hospitalizations. J Am Coll Cardiol. 2023;81(suppl 8):1796. doi:10.1016/S0735-1097(23)02240-4
4. Thotamgari SR, Babbili A, Sheth A, Grewal U, Dani SS, Ganatra S. Racial disparities in hospitalizations for acute heart failure in patients with cancer treatment-related cardiac dysfunction. J Am Coll Cardiol. 2023;81(suppl 8):2391. doi:10.1016/S0735-1097(23)02835-8
5. Golec S, Mitrani L, Yoon J, Dangayach N, Sahni GD. Triple-M (myocarditis-myositis-myasthenia gravis) syndrome in a patient receiving nivolumab: a cardio-oncologic emergency. J Am Coll Cardiol. 2023;81(suppl 8):3459.
doi:10.1016/S0735-1097(23)03903-7
Articles in this issue
almost 3 years ago
From the Editor in Chief: So Far, So Fast, and Yet So Far to Goalmost 3 years ago
Clinical Updates: Spring 2023almost 3 years ago
Managed Care Updates: Spring 2023almost 3 years ago
Recent FDA Actions: Spring 2023almost 3 years ago
Coverage From the 2023 COA Community Oncology Conferencealmost 3 years ago
Coverage From ACCC 2023 Spring Business Summitalmost 3 years ago
Health Equity Coverage: April 2023Newsletter
Stay ahead of policy, cost, and value—subscribe to AJMC for expert insights at the intersection of clinical care and health economics.