
COVID-19 created a striking rise in telehealth services over the past year, as seen in claims tracked by FAIR Health.

COVID-19 created a striking rise in telehealth services over the past year, as seen in claims tracked by FAIR Health.

Although half of US rheumatologists have patients for which nonmedical switching has been suggested, only 35% were likely to switch patients with rheumatoid arthritis doing well on a reference product to a biosimilar.

Intravenous diuretic treatment of patients with decompensated heart failure can increase urine output, promote weight loss, and improve dyspnea.
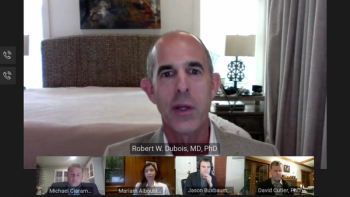
During a webinar, experts discussed where health care has improved life expectancy and the relationship between cost and relative contribution that each area makes to life improvement and expectancy.

To mark the 25th anniversary of The American Journal of Managed Care®, each issue in 2020 will include a special feature: an interview with a thought leader in the world of health care and medicine. The November issue features a conversation with William H. Shrank, MD, MSHS, chief medical officer of Humana.

The patients must always come first, emphasized Milena Murray, PharmD, MSc, BCIDP, AAHIVP, associate professor at Midwestern University College of Pharmacy, who practices at the Northwestern Medicine Infectious Disease Center in Chicago.

Study results demonstrate the multimillion-dollar savings achieved among patients with heart failure with reduced ejection fraction (HFrEF) following treatment initiation with sacubitril and valsartan.

Pharmacists have an important role to play in the success of value-based payment models, according to panelists who discussed their health plan’s value initiatives at the Academy of Managed Care Pharmacy Nexus 2020 meeting.

In a panel discussion at the Academy of Managed Care Pharmacy Nexus 2020 meeting, experts discussed driving factors of and barriers to the use of real-world evidence by payers in oncology decision-making.

As the coronavirus disease 2019 (COVID-19) pandemic threatens to worsen the opioid crisis, payers must rapidly deploy policies to ensure care for individuals with opioid use disorder.

The authors, from RxCrossroads by McKesson, discuss the impact of copay accumulator and maximizer programs.

A new national study is highlighting disparities in morbidity and barriers to care that face patients with chronic obstructive pulmonary disease (COPD) living in in rural areas.

Natera’s Signatera ctDNA test will determine study eligibility and treatment effectiveness in HR-positive, HER2-negative breast cancer patients.

More Humana doctors are taking on full global risk under Medicare Advantage than are still using traditional fee-for-service.

The relatively few examples of commercially funded condition-specific bundled payments provide insights into how to spread this alternative payment model further in the private insurance market.

More biosimilars are hitting the US market, but marketplace dynamics have made it difficult to take advantage of these therapies.

Pediatric patients who had a referral from their pediatric rheumatologist and continued insurance coverage saw decreased delays when transitioning to an adult rheumatology clinic.
Trump administration officials said the new payment incentives represent the biggest change in kidney care in decades.

The authors used health care claims and survey data to identify a strategy that might promote life satisfaction while advancing equity in an insured population.

A FAIR Health review finds a dramatic drop in dental claims in March and April 2020 due to COVID-19.

Reports of Medicare Advantage (MA) patients receiving higher-quality care for their cardiovascular disease prompted this comparison study of patients with heart failure enrolled in Medicare fee-for-service plans (FFS) and MA plans.

A decision-analytic model could save more than $7 million in overall ineffective health care costs per 1000 patients by predicting which patients with rheumatoid arthritis (RA) will have an inadequate response to anti–tumor necrosis factor therapies.
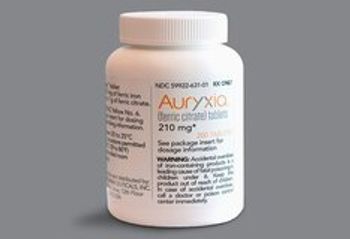
Members of Congress introduce a bill to force Medicare to cover a drug they say will protect CKD patients during the COVID-19 pandemic.

Telehealth claim lines increased 4132% nationally from June 2019 to June 2020, rising from 0.16% of medical claim lines in June 2019 to 6.85% in June 2020, according to new data from FAIR Health’s Monthly Telehealth Regional Tracker.

Data presented during the European Society for Cardiology 2020 Congress were a follow-up to the presentation of VERTIS CV at the American Diabetes Association Scientific Sessions in June.

259 Prospect Plains Rd, Bldg H
Cranbury, NJ 08512
© 2025 MJH Life Sciences®
All rights reserved.
